
The traditional healthcare model has long functioned as a reactive cleanup crew that only arrives after the house is already on fire, but the ORIGIN project is finally handing us the blueprints to detect the very first spark before it even ignites a flame. This landmark initiative represents a

Modern medicine often forces patients with systemic lupus erythematosus into a difficult trade-off between managing life-threatening organ damage and enduring the harsh, systemic toxicity of long-term steroid use. While existing treatments offer some relief, they frequently fail to address the

The subtle tremor in a hand or a slight change in vocal pitch often serves as the first whisper of a neurological condition that remains one of the most challenging puzzles for modern clinicians. Parkinson’s disease presents a complex diagnostic landscape where symptoms are frequently subtle,

The conventional method of determining a pregnancy's timeline has remained largely unchanged for nearly two centuries, relying on a mix of patient memory and rudimentary calculations that often miss the mark by weeks. For decades, pregnancy dating has functioned as an educated guess rather than a
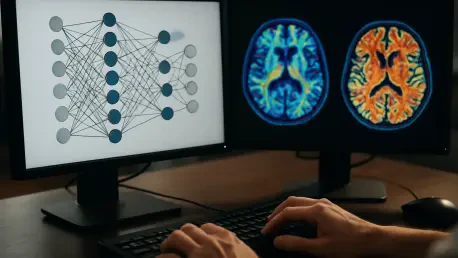
The High Stakes of the Alzheimer’s Waiting Game A diagnosis of Alzheimer’s Disease often feels like being handed a map with the ink still wet, leaving families to navigate a landscape where the landmarks of memory and independence could vanish tomorrow or remain for a decade. This profound
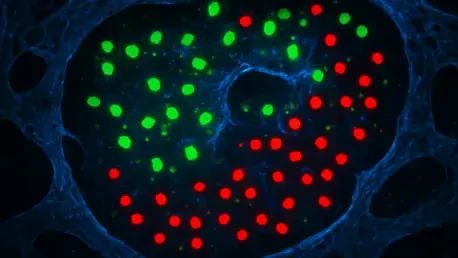
Scientists have successfully mapped the internal genetic blueprints of millions of individual cells, yet the precise physical coordinates of these cells within the living architecture of an organ often vanish the moment they are extracted for study. This "spatial gap" has long hindered the ability
1 2 3 4 5 6 7 8 9 10 11 12 13 14 15 16 17 18 19 20 21 22 23 24 25 26 27 28 29 30 31 32 33 34 35 36 37 38 39 40 41 42 43 44 45 46 47 48 49 50 51 52 53 54 55 56 57 58 59 60 61 62 63 64 65 66 67 68 69