For millions of women, the annual or biennial mammogram is a familiar, if sometimes uncomfortable, part of their preventive health routine—a critical tool in the ongoing fight against breast cancer. A comprehensive analysis of recent medical research highlights the significant, yet largely underutilized, potential of routine mammography as a predictive tool for cardiovascular disease, the leading cause of mortality in adults. This routine screening, long valued for its ability to detect malignancies, may hold the key to identifying another, often silent, threat to women’s health. The story lies not in the breast tissue itself, but within the arteries that supply it. A growing body of evidence shows that calcium deposits in these vessels, a condition known as Breast Arterial Calcification (BAC), are a powerful indicator of systemic vascular disease. This finding is particularly crucial because heart disease presents differently and often more subtly in women, leading to diagnostic delays and poorer outcomes. Leveraging a test that is already widely performed offers a groundbreaking opportunity to close this gap without additional procedures, costs, or radiation exposure, transforming a cancer screening into a dual-purpose lifesaver.
The Unseen Warning in a Routine Screening
The potential for mammography to serve a dual purpose represents a significant advancement in preventive medicine. Its primary role in breast cancer detection is well-established and has saved countless lives through early diagnosis. However, the incidental findings on these X-ray images, specifically the calcification within arterial walls, have long been noted but largely dismissed as irrelevant to breast health. Researchers are now reframing these observations not as incidental but as invaluable clues to a woman’s overall cardiovascular condition.
This shift in perspective is driven by an urgent need for better diagnostic tools for women. Cardiovascular disease remains the leading cause of death for women globally, yet the path to diagnosis is often fraught with challenges. Symptoms can be atypical compared to the classic chest-clutching presentation more common in men, leading to misdiagnosis or delayed treatment. By identifying a reliable biomarker on an existing screening test, clinicians could gain a crucial early warning sign, prompting timely intervention for a condition that might otherwise go unnoticed until a catastrophic event occurs.
A Critical Blind Spot in Women’s Heart Health
A persistent disparity exists in cardiovascular outcomes between genders. Women are frequently diagnosed at more advanced stages of heart disease and, consequently, face a worse prognosis after events such as a heart attack or stroke. This troubling trend is partially rooted in the limitations of traditional risk-assessment models, which were developed based on studies that predominantly included male participants and may not accurately capture the unique risk factors and disease progression in women. This gap in knowledge underscores the necessity for more gender-specific and accessible screening methods.
While advanced imaging like a coronary CT scan can directly measure calcium in the heart’s arteries, it is not a routine screening tool for the general population. Significant barriers, including the financial cost of the procedure and patient concerns about radiation exposure, limit its widespread use. A CT scan is typically recommended only after other risk factors have been identified. Mammography, in contrast, is an established part of preventive care for millions of women over 40, presenting a unique and readily available resource for opportunistic cardiovascular risk assessment that circumvents these common obstacles.
Decoding the Image for Breast Arterial Calcification
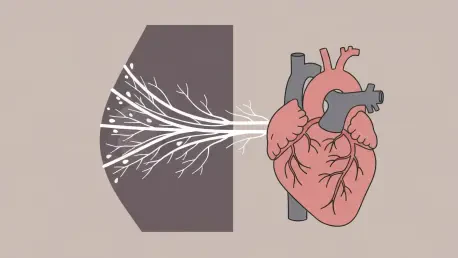
At the heart of this discovery is Breast Arterial Calcification, or BAC. This condition refers to the accumulation of calcium deposits along the middle layer of the breast’s arterial walls, which appear as distinct, track-like white lines on a standard mammogram. While these calcifications are located in the breast, they are not associated with breast cancer risk. Instead, they are a manifestation of atherosclerosis, the same underlying process of hardening and narrowing of the arteries that leads to heart attacks and strokes elsewhere in the body.
The presence of BAC serves as a powerful, yet historically overlooked, biomarker for systemic vascular health. Because the arteries in the breast reflect the condition of arteries throughout the body, identifying calcification here provides a window into a patient’s broader cardiovascular risk. This allows for what experts call “opportunistic screening”—the ability to extract vital secondary information from a test performed for another primary reason. This approach leverages an existing healthcare infrastructure to provide immense value at no additional cost, time, or radiation dose to the patient.
New Research Quantifies the Stark Connection
Compelling new evidence solidifying this link was presented at a recent meeting of the Radiological Society of North America. A groundbreaking study led by Dr. Matthew Nudy, an assistant professor at Penn State College of Medicine, moved beyond simply noting the presence of BAC to meticulously quantifying its severity and, most importantly, its progression over time. This longitudinal approach has provided the most robust data to date on the predictive power of this biomarker.
The research team conducted a large-scale retrospective analysis of over 10,000 women who had undergone sequential mammograms. Using an advanced, investigational artificial intelligence (AI) software, the team measured the extent of arterial calcification on each image, allowing them to track changes with precision. The findings were striking. Women in the most severe BAC category at their initial screening had up to double the risk of a major cardiovascular event. However, the most potent predictor was the rate of change; tracking the progression of calcification over time proved to be a more critical factor than a single static measurement.
The statistical significance of these findings cannot be overstated. The study revealed that women whose calcification worsened between screenings faced a dramatically elevated risk. For instance, those who progressed from a “moderate” to a “severe” level of calcification saw their risk for an adverse event or death escalate by a staggering 93%. Even developing mild calcification where there was none before increased risk by 41%. These numbers provide a clear, quantifiable connection between what is seen on a mammogram and a woman’s future heart health.
From Image to Action in Clinical Practice
These robust findings are prompting a call for a fundamental change in how mammogram results are interpreted and reported. Currently, BAC is often not mentioned in radiology reports because it has no bearing on breast cancer. Dr. Nudy and other experts argue that this needs to change. “This could be a way to use data that may already be available for a different reason and to potentially use it to risk-stratify an individual for the development of cardiovascular disease,” he stated, emphasizing the untapped potential of existing medical images.
The clinical applications are profound and immediate. Including a standardized assessment of BAC in every mammogram report could trigger crucial, early conversations between patients and their physicians about heart health. For a woman identified with moderate or progressing BAC, this finding could be the catalyst for preventive strategies, ranging from aggressive lifestyle modifications like diet and exercise to the initiation of cholesterol-lowering medication or a recommendation for further, more specific cardiac testing.
The path forward requires the development and adoption of standardized protocols for radiologists to assess and report BAC consistently. Integrating this information seamlessly into patient care workflows is the next critical step. By turning a routine image into a proactive tool for risk stratification, the medical community can empower women with invaluable knowledge about their cardiovascular health, potentially preventing devastating cardiac events for years to come.
The culmination of this research marked a pivotal moment in women’s preventive healthcare. The evidence firmly established that the faint white lines of calcification on a mammogram were not merely incidental artifacts but direct indicators of a silent and progressive systemic disease. It was clear that by systematically reporting on Breast Arterial Calcification, radiologists could provide clinicians with a powerful, no-cost tool to initiate lifesaving conversations and interventions. This simple shift in practice promised to transform a routine cancer screening into a frontline defense against the leading cause of death in women, bridging a long-standing gap in cardiovascular risk assessment and heralding a more integrated and proactive approach to health.