The emergence of highly pathogenic avian influenza (HPAI) H5N1 in 1996 marked a significant event in the history of infectious diseases. Over the years, this virus has spread across continents, infecting various species and creating diverse clades. The potential for H5N1 to adapt to humans through key mutations has become a critical area of research, especially with recent outbreaks in bovine populations. This investigation into receptor-binding adaptations and specific mutations is crucial in understanding the virus’s capability to infect humans and highlights the need for vigilant monitoring.
Historical Context and Emergence of H5N1
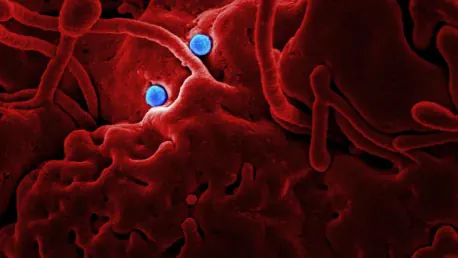
The H5N1 virus first emerged in 1996 and quickly spread across Asia, Europe, and Africa, causing significant outbreaks in poultry and wild birds. This virus is known for its high pathogenicity and ability to infect multiple species, including humans. Given its virulence and cross-species transmission, H5N1 posed a serious threat to both animal and human health. Over the years, numerous clades of the virus have emerged, each exhibiting unique genetic variations that complicate efforts to control the virus and prevent outbreaks.
In late 2021, a new clade, 2.3.4.4b, emerged in North America, leading to infections in avian species, mammals, and even humans. This development raised concerns about the virus’s potential to adapt to human hosts and cause a pandemic. The detection of bovine H5N1 infections in the United States dairy herds in 2024, leading to the first recorded human cases of bovine H5N1 infections, further underscores the need for vigilance and continued research into these mutations. These incidents illuminate the persistent and evolving threat posed by H5N1 and its potential for broader zoonotic transmission.
Recent Developments in Bovine H5N1 Infections
The first human cases of bovine H5N1 infections were reported in 2024, following an outbreak in dairy herds in the United States. Genetic analysis of the virus from these bovine-origin infections revealed potential adaptations in the hemagglutinin (HA) receptor-binding domain that could facilitate human infections. This revelation is particularly significant as it highlights the virus’s ability to mutate and adapt, thus enhancing its potential to cross species barriers and pose public health risks.
Researchers have intensely focused on the HA ectodomain sequence from the influenza A/Texas/37/2024 H5N1 virus, sourced from the Global Initiative on Sharing All Influenza Data (GISAID). By employing various biochemical assays and chromatography techniques, scientists have been able to analyze the binding preferences of the virus HA and identify key mutations that may enhance its ability to infect humans. This thorough investigation aims to decode the viral behavior at the molecular level, providing insights necessary for devising strategic interventions and mitigating potential outbreaks.
Experimentation and Research Methodology
To investigate the potential for human adaptation, researchers cloned the HA sequence into a pFastbac-1 vector and expressed it in cells. The purified protein was then subjected to structural studies and receptor-binding assays using advanced techniques such as surface plasmon resonance (SPR), enzyme-linked immunosorbent assay (ELISA), and glycan microarrays. These sophisticated methods enabled a detailed analysis of the virus’s binding preferences and the impact of specific mutations, shedding light on the virus’s adaptability and the associated risks.
The wild-type (WT) bovine Texas H5 HA demonstrated a strong preference for avian receptors (α2-3 sialosides) and no detectable binding to human receptors (α2-6 sialosides). This data suggests that the virus, in its present form, is not inherently adapted to infect humans. However, the introduction of the Gln226Leu mutation in the receptor-binding site of Texas H5 HA completely switched the specificity from avian to human-type receptors. This pivotal finding indicates how a single mutation can drastically alter viral behavior and highlight the importance of understanding these genetic shifts.
Key Findings and Implications
The Gln226Leu mutation significantly enhanced the virus’s ability to bind to human receptors compared to the wild-type strain. This mutation mirrors the receptor-binding characteristics of transmissible human influenza viruses, indicating a potential pathway for zoonotic adaptation. Such mutations represent a mechanism through which the virus can evolve to better infect human hosts, thus heightening the risk of cross-species transmission and potential pandemics. Additional mutations, such as Asn224Lys combined with Gln226Leu, further improved the binding affinity to human receptors, emphasizing the virus’s complex capacity for adaptation.
Structural analysis through crystallization provided further insights into the molecular interactions responsible for the shift in receptor specificity. The altered interactions, such as van der Waals interactions formed by leucine in the Gln226Leu mutation, underscore the importance of these mutations in facilitating human adaptation. These structural modifications at the molecular level signify the virus’s gradual but impactful adjustments toward becoming more adept at infecting human cells, warranting urgent attention from the global health community.
Overarching Trends and Consensus Viewpoints
The spread of clade 2.3.4.4b H5N1 viruses in recent years has raised significant concerns about their potential to cause a pandemic. The ability of these viruses to infect a range of species, including humans, underscores the need for ongoing surveillance and research. Key mutations, such as Gln226Leu, demonstrate the virus’s potential to adapt to human hosts, emphasizing the importance of detailed genetic analysis and monitoring emerging strains. This ongoing research forms the cornerstone of efforts to preempt and combat potential outbreaks, thereby safeguarding public health on a global scale.
The findings from recent studies suggest that while the bovine H5 HA primarily binds avian receptors, certain mutations can significantly shift its preference to human receptors. This potential for zoonotic adaptation highlights the critical need for global monitoring and preparedness to mitigate the risks posed by emerging influenza strains with pandemic potential. By understanding the patterns and trends in viral mutation, health organizations can better strategize their response, enhancing both prevention and intervention measures.
Methodological Approach and Binding Assay Results
The emergence of highly pathogenic avian influenza (HPAI) H5N1 in 1996 was a pivotal event in the history of infectious diseases. Over the years, this virus has spread to various continents, affecting a multitude of species and developing numerous clades, or subtypes. Notably, the H5N1 virus has the potential to adapt to humans through key genetic mutations, which has become a significant area of research.
Recent outbreaks of H5N1 in bovine populations have heightened the urgency of this research, as these mutations could potentially make the virus more capable of infecting humans. Scientists are particularly focused on studying the virus’s receptor-binding adaptations and specific genetic changes that could facilitate this cross-species transmission.
Understanding how H5N1 could evolve to infect humans is not just a theoretical exercise; it’s a necessity for public health. This research highlights the importance of continuous and vigilant monitoring of the virus, to prevent possible human pandemics. As H5N1 continues to evolve, so too must our strategies for surveillance, preparedness, and response. Constant vigilance and research are essential to mitigate the risks posed by this potentially deadly virus.