At the beginning of the COVID-19 pandemic, people around the world were comparing the new disease with the flu, also known as influenza. However, while both diseases cause respiratory symptoms, it soon became very clear that there are some important differences between them, as well as between the two viruses that cause them. Another disease caused by a virus is now rapidly spreading throughout the world, and with monkeypox becoming a challenge in the U.S. and abroad, more and more people are comparing the disease with another scourge that terrorized mankind for centuries: smallpox.
Now eradicated, smallpox was once a terrible threat to people everywhere, killing hundreds of millions through the centuries. While the origin of the virus that caused it remains obscure, the World Health Organization (WHO) declared the disease eradicated in 1980. Scientists are still studying smallpox and the deadly virus that causes it, with new vaccines and treatments still being created. Some of these are now used against monkeypox, while others will most likely be used to prevent future pandemics.
The History of Vaccination Begins with Smallpox
Smallpox has been a terrible threat for humanity over the last 1500 years, although it could go back even further. Ancient Greek sources do not mention this menacing disease, but writings from the Roman Empire do mention pustular diseases with symptoms similar to those of smallpox. According to the WHO, Edward Jenner developed the smallpox vaccine in 1796 after he noticed that milkmaids who previously contracted cowpox did not get infected with smallpox or develop symptoms of the disease. His research proved that inoculated vaccinia protected against the variola virus—the virus that causes smallpox.
The vaccine developed by Edward Jenner in 1796 was not only the best prevention method against smallpox available at the time, but also the first vaccine ever created. A modern variant of that vaccine was developed later, in the 1950s, when a new method to produce a heat-stable, freeze-dried vaccine was discovered. This newer variant came with an important advantage: Medical personnel could store the vaccine for longer, even without refrigeration. With the invention of the bifurcated needle in 1961, vaccination became even easier, and smallpox was eradicated in the U.S. by 1972. Routine smallpox vaccination among Americans stopped the same year, according to the Centers for Disease Control and Prevention (CDC).
Fifty years later, the smallpox vaccine is only recommended for lab workers handling a virus that causes smallpox or other similar viruses. It is also recommended in the event of a future smallpox outbreak. However, with the number of monkeypox cases now rising around the world, scientists wonder if the time has come for smallpox vaccines and treatments to play an important role once again.
How Smallpox Vaccines and Treatments Work Against Monkeypox
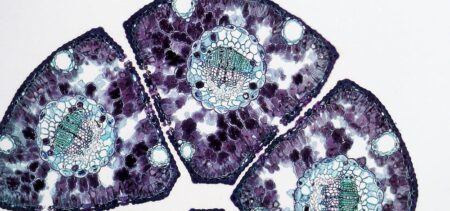
The virus that causes monkeypox is closely related to the one responsible for smallpox, as both are part of the four orthopoxviruses known to cause infectious diseases in humans: variola, vaccinia, cowpox, and monkeypox. This is precisely why the CDC names JYNNEOS, also known as Imvamune or Imvanex, as the only attenuated live virus vaccine approved by the U.S. Food and Drug Administration for the prevention of monkeypox. This vaccine was developed to ensure that all Americans can be protected from smallpox, as well as monkeypox, in spite of the fact that this disease was eradicated 50 years ago. Because the U.S. stashed vaccines in the event of an outbreak, health officials were able to send almost 1,200 vaccine doses to those in need as soon as 21 Americans became infected with monkeypox.
Similarly, scientists from the United Kingdom decided to use a treatment drug initially developed for smallpox to treat a person suffering from monkeypox in 2021. The drug was shown to shorten the duration of the disease when compared to other similar cases. Scientist Hugh Adler from the Liverpool School of Tropical Medicine later said that, despite the fact that the new drug was only administered to one patient, the result can be seen as “a signal that Tecovirimat is a promising drug and should be taken forward for studies.” Like Tecovirimat, other treatments previously developed to treat smallpox and other diseases are now available in the U.S. as monkeypox treatments: Cidofovir (also known as Vistide) and Vaccinia Immune Globulin Intravenous, or VIGIV. The CDC is also currently developing an Expanded Access Investigational New Drug Application for Brincidofovir.
Like COVID-19, monkeypox is undoubtedly a challenge that will test healthcare systems, as well as treatments and therapeutic interventions in the U.S. and abroad. However, unlike the recent pandemic and unlike smallpox throughout the ages, the current monkeypox outbreak poses only a moderate risk to global public health according to the WHO. One of the reasons for this statement might be the fact that smallpox research had led to the development of vaccines and treatments that can now be used to treat monkeypox.