Imagine a child struggling with unexplained neurological symptoms, leaving doctors puzzled and families desperate for answers, only to discover that MPV17-related mitochondrial DNA depletion syndrome (MDDS), a rare genetic disorder caused by mutations in the MPV17 gene, often lies at the heart of such mysteries. This condition disrupts mitochondrial function, leading to energy deficits in critical organs like the brain and liver, with devastating consequences. For those affected, the diagnostic journey can be long and frustrating, but magnetic resonance imaging (MRI) has emerged as a pivotal tool in uncovering the hidden effects of this syndrome. By revealing specific brain abnormalities tied to MPV17 mutations, MRI offers a lifeline for early detection and tailored care. This article explores the distinct MRI signs associated with this disorder, shedding light on how they guide clinicians in navigating a complex diagnosis. Understanding these imaging markers not only aids in identifying the condition but also paves the way for better management and hope for affected families.
Decoding Brain Changes Through MRI Technology
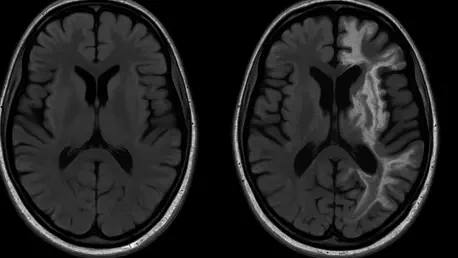
MRI technology has revolutionized the approach to diagnosing MPV17-related MDDS by providing a clear window into the brain’s structure. Research highlights that this syndrome often manifests as distinct alterations in cerebral white and gray matter, which play essential roles in neural communication and processing. These changes, though sometimes subtle, become visible through high-resolution imaging, serving as critical indicators for clinicians. Recognizing these patterns allows for a quicker and more precise diagnosis, even when a patient’s symptoms are ambiguous or overlap with other neurological conditions. The ability of MRI to detect such specific markers transforms it into an indispensable asset in the medical field, particularly for rare disorders where traditional diagnostic methods may fall short. This clarity is especially vital in pediatric cases, where early identification can significantly influence long-term outcomes and quality of life.
Beyond merely identifying abnormalities, MRI offers insights into the extent and location of brain changes caused by MPV17 mutations. It can reveal whether the damage is localized to certain areas or more widespread across neural tissues, providing a detailed map of the syndrome’s impact. This information is crucial for assessing the severity of the condition and helps clinicians predict potential complications, such as cognitive or motor impairments. With this level of detail, healthcare providers can design individualized treatment plans that address the unique challenges faced by each patient. The precision of MRI ensures that interventions are not based on guesswork but on concrete evidence of the brain’s condition, fostering a more targeted and effective approach to care. This diagnostic precision ultimately reduces the uncertainty that often accompanies rare genetic disorders, offering a clearer path forward for both medical teams and families.
Age-Related Differences in MRI Findings
The presentation of MRI signs in MPV17-related MDDS varies significantly across different age groups, adding a layer of complexity to diagnosis. In younger children, brain abnormalities might appear faint or underdeveloped, often requiring specialized imaging techniques to detect. As these children grow, the changes can become more apparent, reflecting the progressive nature of mitochondrial dysfunction. This age-dependent variability underscores the importance of conducting MRI scans at multiple stages of development, particularly for those with early signs of neurological issues. For clinicians, understanding that these markers may evolve over time is key to avoiding misdiagnosis and ensuring that subtle early indicators are not overlooked. Regular imaging becomes a vital strategy in tracking the syndrome’s progression and adapting care as needed.
In adolescents, MRI findings often reveal more pronounced abnormalities, as years of mitochondrial impairment take a cumulative toll on brain structures. These changes might include more extensive white matter disruptions or gray matter atrophy, pointing to a higher risk of severe neurological decline. This progression highlights why early MRI screening is so critical—identifying issues in childhood can lead to interventions that mitigate damage before it becomes irreversible. For families with at-risk children, this knowledge emphasizes the need for proactive monitoring and collaboration with healthcare providers. The age factor in MRI results serves as a reminder that MPV17-related MDDS is not a static condition but one that evolves, requiring ongoing vigilance and adaptability in both diagnosis and management to safeguard long-term health.
Impact of MRI Signs on Clinical Management
The specific MRI signs associated with MPV17-related MDDS play a transformative role in shaping clinical management strategies. When imaging reveals particular changes in white matter, for instance, it might indicate an elevated risk of motor difficulties or cognitive delays, prompting the early introduction of physical therapy or specialized educational support. These findings enable healthcare teams to monitor the condition’s progression over time, adjusting interventions to address emerging challenges as they arise. MRI thus acts as a dynamic tool, ensuring that care remains responsive to the patient’s current needs rather than relying on outdated assumptions. This tailored approach can significantly improve outcomes, especially in mitigating the long-term effects of neurological damage in young patients facing this rare disorder.
Additionally, the clarity provided by MRI results offers substantial emotional relief to families navigating the uncertainties of a rare genetic condition. Seeing concrete evidence of brain changes can replace vague fears with actionable steps, helping parents and caregivers better understand what lies ahead. This diagnostic precision reduces the frustration of unexplained symptoms and fosters a sense of direction in managing the syndrome. For medical professionals, these imaging insights also facilitate better communication with families, ensuring that complex medical information is conveyed in a way that empowers rather than overwhelms. The integration of MRI into routine care for suspected MPV17 cases thus enhances not only clinical decision-making but also the overall support system surrounding affected individuals.
Exploring Future Possibilities Through Imaging Insights
MRI findings in MPV17-related MDDS are not just diagnostic tools but also gateways to advancing scientific understanding of mitochondrial disorders. By correlating specific brain abnormalities with genetic mutations in the MPV17 gene, researchers can delve deeper into the metabolic disruptions at the core of this condition. This connection offers a promising avenue for identifying potential therapeutic targets, such as interventions that might protect or restore mitochondrial function. The detailed imagery provided by MRI scans contributes to a growing body of knowledge, helping scientists piece together the intricate puzzle of how genetic flaws translate into physical symptoms. Such insights are essential for developing innovative treatments that could one day slow or even halt the progression of this debilitating syndrome.
Furthermore, the implications of these MRI signs extend to the broader field of precision medicine, where treatments are customized to individual genetic and clinical profiles. The ability to detect and analyze brain changes through imaging supports the push for routine genetic screening in at-risk populations, ensuring that diagnoses are made before significant damage occurs. This proactive stance, bolstered by interdisciplinary collaboration among geneticists, neurologists, and radiologists, holds the potential to transform how mitochondrial disorders are managed. As each MRI scan adds to the collective understanding, it fuels hope for breakthroughs that could improve outcomes for patients and ease the burden on families. The journey from imaging to innovation reflects a commitment to turning scientific discovery into tangible benefits for those affected by rare conditions.
Reflecting on Progress and Next Steps
Looking back, the identification of MRI signs in MPV17-related mitochondrial DNA depletion syndrome marked a significant stride in tackling a once-elusive disorder. The detailed imaging of cerebral white and gray matter abnormalities provided clinicians with a reliable framework for diagnosis, while early detection paved the way for timely interventions. Collaborative efforts among medical fields enriched the approach to care, ensuring that patients received comprehensive support tailored to their needs. As research unfolded, these MRI insights laid a strong foundation for exploring the metabolic and genetic underpinnings of the condition. Moving forward, the focus should shift to translating these findings into novel therapies, expanding genetic screening programs, and fostering global partnerships to share knowledge. Continued investment in advanced imaging and interdisciplinary studies will be crucial to unlocking new solutions, ensuring that hope for better outcomes remains a driving force in the fight against mitochondrial disorders.