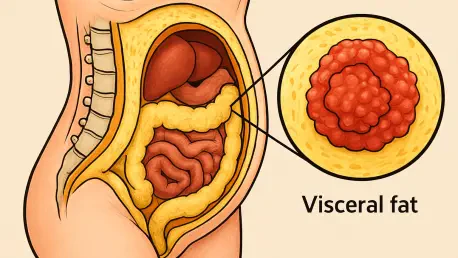
A startling revelation from a recent study conducted in Norway has brought new attention to the hidden dangers lurking within the body, specifically the role of visceral fat in driving the severity of endometrial cancer, a finding that underscores the urgent need for refined risk assessment. This type of fat, which envelops vital internal organs, has long been associated with various health risks, but its metabolic activity is now emerging as a critical factor in determining cancer aggressiveness. Unlike subcutaneous fat that lies just beneath the skin, visceral fat exerts a profound influence on systemic inflammation and metabolism, potentially fueling tumor growth. Presented at a prominent European medical congress, this research challenges conventional metrics like body mass index (BMI) and shifts the focus toward a deeper understanding of fat’s biological behavior. As obesity remains a significant risk factor for numerous cancers, these findings highlight an urgent need to refine how risks are assessed and managed in clinical settings, paving the way for more tailored approaches to treatment.
Unveiling the Metabolic Connection
Groundbreaking research from a Norwegian team at the University of Bergen has illuminated a compelling link between the metabolic activity of visceral fat and the progression of endometrial cancer. The study, involving 274 women at Haukeland University Hospital, utilized advanced imaging techniques such as positron emission tomography-computed tomography (PET-CT) to measure glucose uptake in visceral fat as an indicator of its metabolic behavior. The results were striking: women exhibiting higher metabolic activity in this fat type were far more likely to have advanced stages of the disease and lymph node metastases. This discovery suggests that it’s not merely the amount of visceral fat that matters, but rather how active it is at a cellular level. Such insights challenge the long-standing reliance on BMI as the primary gauge of obesity-related cancer risk, pointing instead to the importance of qualitative assessments of fat tissue in predicting patient outcomes and shaping clinical strategies.
Beyond the numbers, the study’s findings reveal a nuanced perspective on how visceral fat influences cancer severity through intricate biological pathways. While the volume of visceral fat showed little correlation with its metabolic activity, the latter emerged as a key driver of disease progression. Researchers noted that metabolically active visceral fat may create an environment conducive to tumor growth by releasing specific signaling molecules and fostering chronic inflammation. This inflammatory state can disrupt normal cellular functions, potentially accelerating cancer spread to surrounding tissues like lymph nodes. Moreover, the study aligns with prior research from the same institution, which identified visceral fat percentage as a stronger predictor of poor prognosis compared to traditional metrics. This shift in focus toward fat metabolism offers a fresh lens through which to view obesity’s impact on cancer, urging medical professionals to reconsider how risk factors are evaluated in patients diagnosed with endometrial cancer.
Biological Mechanisms at Play
Delving deeper into the science, the Norwegian study highlights the complex role visceral fat plays in promoting aggressive cancer through multiple biological mechanisms. Unlike the relatively inert subcutaneous fat, visceral fat is highly active, significantly impacting whole-body metabolism and inflammation. The research suggests that chronic inflammation within visceral fat releases cytokines and fatty acids, which can directly contribute to tumor development and help cancer cells evade immune detection. Additionally, this inflammatory environment may lead to insulin resistance, a well-documented risk factor for cancer progression. These interactions create a vicious cycle, where visceral fat not only supports tumor growth but also amplifies systemic conditions that exacerbate disease severity. Such findings emphasize that visceral fat’s influence extends beyond endometrial cancer, linking it to broader health issues like cardiovascular disease and type 2 diabetes, thus warranting a comprehensive approach to patient care.
Another critical aspect uncovered by the research is the role of adipokines—signaling molecules produced by fat tissue—and their interaction with tumor cells in driving cancer spread. These molecules, along with direct cellular crosstalk between visceral fat and cancerous tissues, are believed to facilitate metastasis, particularly to lymph nodes, a hallmark of advanced disease stages. The study’s insights suggest that visceral fat acts as more than just a passive energy store; it’s an active participant in creating a pro-cancer environment through hormonal and inflammatory pathways. This multifaceted relationship underscores why targeting visceral fat metabolism could be a game-changer in managing not just endometrial cancer but other obesity-related conditions. By understanding these mechanisms, researchers are better positioned to develop interventions that disrupt these harmful interactions, potentially slowing disease progression and improving survival rates for affected patients.
Clinical Implications and Future Directions
The implications of this Norwegian study for clinical practice are profound, offering a potential pathway to identify high-risk endometrial cancer patients through visceral fat metabolism assessments. By using imaging techniques like PET-CT to detect heightened metabolic activity in visceral fat, physicians could stratify patients more effectively and tailor treatment plans to individual needs. This approach marks a significant departure from generic risk assessments based solely on BMI, moving toward precision medicine that accounts for the unique biological characteristics of each patient’s fat tissue. However, integrating such advanced imaging into routine clinical workflows presents technical challenges, including the need for standardized protocols and accessible technology. Addressing these hurdles will be crucial to ensure that the benefits of this research translate into tangible improvements in patient care and outcomes across diverse healthcare settings.
Looking ahead, the research team is committed to refining these imaging methods and exploring innovative solutions like artificial intelligence (AI) algorithms to enhance patient stratification. Future studies will also investigate the relationship between visceral fat metabolism and blood biomarkers, such as cytokines or hormones, to uncover additional layers of disease interaction. Moreover, tracking changes in fat activity over time could provide valuable insights into how these dynamics influence treatment response and disease progression. These ongoing efforts reflect a broader commitment to bridging the gap between research and real-world application, ensuring that cutting-edge discoveries lead to practical tools for clinicians. As these advancements unfold, they promise to redefine how obesity-related cancer risks are monitored, setting a new standard for personalized care that prioritizes metabolic insights over outdated metrics.
Pioneering a New Era in Cancer Care
Reflecting on the strides made, this study from Norway stands as a pivotal moment in unraveling the intricate ties between visceral fat metabolism and endometrial cancer severity. It demonstrates that women with elevated metabolic activity in visceral fat face a higher likelihood of advanced disease stages and lymph node involvement, driven by inflammatory and hormonal factors. By challenging the adequacy of traditional measures like BMI, the research advocates for sophisticated imaging to pinpoint at-risk patients and customize interventions. Although obstacles in routine implementation persist, the dedication to refining techniques and incorporating AI marks a hopeful path forward. These efforts underscore a transformative shift in cancer management, emphasizing the power of metabolic insights to enhance monitoring and treatment strategies. As the medical community builds on these findings, the focus remains on developing actionable tools and fostering nuanced approaches to improve patient outcomes in the evolving landscape of oncology.