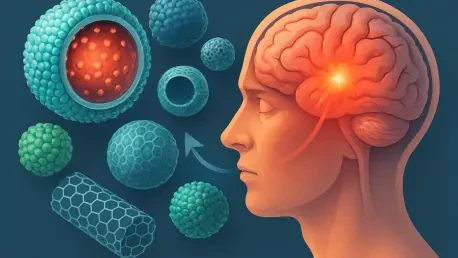
What happens when a traumatic brain injury (TBI) strikes, leaving millions grappling with invisible damage that traditional medicine struggles to detect or treat? In emergency rooms and clinics worldwide, this silent epidemic affects over 60 million people annually, often leading to lifelong disability. Yet, a groundbreaking solution is emerging from the labs—theranostic nanomaterials, tiny engineered particles that promise to both diagnose and heal brain injuries with unprecedented precision. This innovation could redefine how TBI is managed, offering hope where conventional methods fall short.
The significance of this development cannot be overstated. With TBI contributing to a staggering global burden—costing economies billions each year in medical expenses and lost productivity—the need for effective interventions has reached a critical point. Theranostic nanomaterials stand at the forefront of this battle, merging diagnostic and therapeutic capabilities into a single system. This dual approach not only addresses the immediate aftermath of brain trauma but also paves the way for personalized recovery plans, making it a game-changer in neurotrauma care.
A New Frontier in Brain Injury Care: Why Now?
The timing for theranostic nanomaterials couldn’t be more urgent. As the incidence of TBI continues to rise due to accidents, sports injuries, and military conflicts, the limitations of current medical tools have become glaringly apparent. Standard imaging often misses subtle brain damage, while treatments struggle to penetrate the brain’s natural barriers, leaving patients vulnerable to long-term complications.
This gap has spurred intense research into nanotechnology, with theranostic materials emerging as a beacon of progress. These microscopic agents are designed to tackle both detection and treatment simultaneously, offering a lifeline to those affected. The push for such innovation reflects a broader shift in healthcare toward precision medicine, where tailored solutions are no longer a luxury but a necessity.
Moreover, the global focus on brain health has intensified, with governments and institutions allocating significant funding to address neurotrauma. This momentum, coupled with rapid advancements in material science, positions theranostic nanomaterials as a timely response to a pressing crisis. The potential to save lives and reduce disability rates drives this field forward with unparalleled urgency.
The Urgent Need for Innovation in TBI Management
Traumatic brain injury remains a formidable challenge, often dubbed a “silent killer” due to its elusive symptoms and devastating outcomes. Millions worldwide suffer from cognitive impairment or chronic pain following an injury, with many cases going undiagnosed for weeks or months. The inadequacy of existing diagnostic methods, such as CT scans, compounds the problem, as they frequently fail to capture early-stage damage.
Therapeutic hurdles are equally daunting, as the blood-brain barrier—a protective shield around the brain—blocks most drugs from reaching affected areas. This barrier, while vital for defense, often renders conventional treatments ineffective, leaving inflammation and oxidative stress unchecked. The result is a vicious cycle of worsening damage that traditional medicine struggles to interrupt.
Enter theranostic nanomaterials, a revolutionary approach that integrates diagnosis and therapy into one cohesive platform. By bypassing biological barriers and delivering targeted interventions, these technologies address the core issues of TBI management. Their ability to provide real-time insights while administering treatment marks a critical step toward minimizing long-term harm and improving patient outcomes.
Unpacking Theranostic Nanomaterials: Key Mechanisms and Applications
At the heart of this innovation lie theranostic nanomaterials, engineered particles typically smaller than a human cell, capable of performing dual roles in TBI care. These materials can cross the blood-brain barrier to deliver neuroprotective drugs directly to damaged tissue, while simultaneously acting as diagnostic tools to monitor injury progression. Their design often incorporates responsive elements that activate in the presence of specific biological signals, such as acidity or oxidative stress, common in injured brain environments.
Specific types of nanomaterials showcase remarkable versatility in this field. Lipid nanoparticles (LNPs), for instance, excel at targeting affected regions and releasing anti-inflammatory agents with precision, reducing swelling that can exacerbate brain damage. Meanwhile, carbon-dot nanozymes mimic natural enzymes to neutralize harmful reactive molecules, protecting healthy tissue from further harm. These applications highlight the potential to address multiple facets of TBI in a single intervention.
Beyond treatment, diagnostic capabilities are equally impressive. Nanosensors, such as peptide-based or biomarker-responsive variants, provide critical data on injury severity by detecting chemical changes in the brain. This real-time feedback allows clinicians to adjust therapies dynamically, ensuring that interventions remain effective as recovery unfolds. Such advancements signal a shift toward a more integrated and responsive approach to neurotrauma care.
Voices from the Field: Expert Insights and Research Breakthroughs
Leading minds in nanotechnology are vocal about the transformative power of theranostic materials. Professor Yun Hak Kim from Pusan National University emphasizes the potential for customization, noting, “These nanomaterials allow treatments to adapt to each patient’s unique injury profile, a leap forward in personalized care.” His research underscores how integrating diagnostic and therapeutic functions can streamline TBI management, reducing the guesswork that often plagues traditional methods.
Recent studies also point to exciting trends, such as the fusion of nanotechnology with artificial intelligence. Early experiments demonstrate that AI-driven platforms can analyze data from nanosensors to adjust treatments in real time, optimizing outcomes for individual patients. While still in developmental stages, these adaptive systems hint at a future where brain injury care is not only precise but also anticipatory, responding to changes before they escalate.
However, caution remains a recurring theme among experts. Safety concerns, particularly around the long-term effects of nanomaterials in the body, are a priority. Research highlights the importance of designing particles that degrade harmlessly, preventing accumulation that could pose health risks. This balance of optimism and vigilance shapes the narrative around theranostic advancements, grounding enthusiasm in practical considerations.
Navigating the Future: Practical Steps for Advancing Theranostic Solutions
Bringing theranostic nanomaterials from laboratory to clinical use demands a clear roadmap. A primary focus should be on developing biodegradable materials that break down safely in response to environmental cues like pH changes or enzyme activity within the brain. Such designs minimize the risk of toxicity, addressing one of the most significant barriers to widespread adoption.
Collaboration between researchers and healthcare providers is also essential to accelerate progress. Clinical trials must be prioritized to test the efficacy of specific nanomaterials, such as lipid nanoparticles or carbon-dot nanozymes, in real-world scenarios. These studies can provide the evidence needed to gain regulatory approval, ensuring that innovations reach patients without unnecessary delays.
Finally, integrating these technologies with digital tools offers a pathway to even greater impact. AI-driven platforms, for instance, could analyze diagnostic data from nanosensors to tailor treatments dynamically over the course of recovery. By fostering partnerships across disciplines—spanning material science, neurology, and technology—stakeholders can build a robust framework for implementing theranostic solutions, ultimately transforming the landscape of TBI care.
Reflecting on a Turning Point
Looking back, the journey of theranostic nanomaterials marked a pivotal chapter in the fight against traumatic brain injury. The ability to diagnose and treat with such precision once seemed out of reach, yet relentless innovation brought this vision closer to reality. Each breakthrough, from lipid nanoparticles to AI integration, reflected a collective determination to address one of medicine’s toughest challenges.
As this era unfolded, the focus shifted toward actionable next steps. Researchers and clinicians were urged to prioritize safety through rigorous testing, ensuring that biodegradable designs became the standard. Policymakers and funding bodies played a crucial role too, as their support was vital for scaling clinical trials and bridging the gap between lab and hospital.
The road ahead demanded sustained commitment to collaboration and innovation. By investing in cross-disciplinary efforts and embracing emerging technologies, the medical community laid the groundwork for a future where TBI no longer meant inevitable disability. This turning point served as a reminder that even the most daunting health crises could be met with ingenuity, offering renewed hope to millions worldwide.