In a remarkable stride forward for cancer diagnostics, a cutting-edge whole-body MRI technique is offering new hope to those battling myeloma, a challenging form of blood cancer, through the collaborative efforts of researchers at The Royal Marsden NHS Foundation Trust and The Institute of Cancer Research in London. This innovative approach is capable of detecting minute traces of cancer that often elude traditional testing methods. The significance of such a breakthrough cannot be overstated, as it promises to enhance the precision of treatment plans and improve patient outcomes. By identifying minimal residual disease with unprecedented accuracy, this technology could redefine how clinicians manage a disease that affects thousands annually. Through a combination of scientific rigor and compelling personal accounts, the profound impact of this diagnostic tool emerges, shedding light on its potential to transform lives and reshape the landscape of cancer care.
Unmatched Precision in Cancer Detection
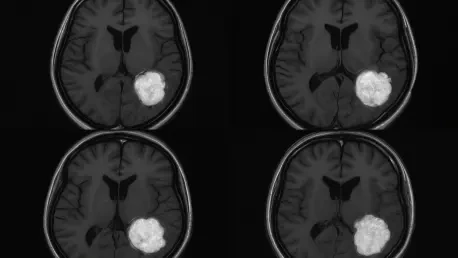
The advent of whole-body MRI marks a pivotal moment in the fight against myeloma, primarily due to its extraordinary ability to detect minimal residual disease (MRD). Traditional diagnostic tools, such as blood tests, bone marrow biopsies, and CT scans, frequently miss small clusters of cancer cells that linger after treatment. In contrast, this advanced imaging technology reveals even the tiniest traces of disease, providing a far more detailed assessment of a patient’s condition. Such precision is invaluable for clinicians striving to evaluate how well a treatment is working and to predict the likelihood of a relapse. By offering a clearer window into the presence of residual cancer, whole-body MRI empowers medical teams to adjust therapeutic strategies proactively, potentially preventing the disease from advancing unnoticed. This level of insight is a cornerstone of modern oncology, where early and accurate detection can significantly alter the trajectory of a patient’s journey.
Further exploring the capabilities of whole-body MRI, its impact extends beyond mere detection to fundamentally enhancing clinical decision-making. Studies involving myeloma patients undergoing stem cell transplants have demonstrated that this technology can identify residual disease in a significant number of cases where other tests show no signs of cancer. Published findings indicate that approximately one in three patients exhibited traces of disease on MRI scans, even when conventional methods suggested remission. Notably, those with positive MRI results often faced shorter overall survival, highlighting the prognostic power of this tool. This ability to correlate imaging data with patient outcomes equips doctors with critical information to tailor interventions more effectively. As a result, whole-body MRI stands as a vital asset in the quest for personalized medicine, ensuring that treatment plans are not only reactive but also predictive in addressing the unique challenges of each case.
A Kinder Approach to Long-Term Monitoring
One of the most compelling advantages of whole-body MRI lies in its patient-friendly design, which prioritizes safety and comfort without compromising on diagnostic accuracy. Unlike many traditional imaging techniques that expose patients to radiation or require invasive procedures like intravenous injections, this method is entirely non-invasive. For individuals with myeloma—a condition often requiring lifelong monitoring due to its chronic nature—this represents a significant relief from the physical toll of repeated testing. The absence of radiation exposure is particularly beneficial, as it eliminates the cumulative risks associated with frequent scans over extended periods. By reducing these burdens, whole-body MRI offers a gentler alternative that aligns with the growing emphasis on patient-centered care in oncology, ensuring that diagnostic processes do not add unnecessary strain to those already facing a challenging disease.
Delving deeper into the benefits for long-term management, whole-body MRI addresses the emotional and logistical challenges faced by myeloma patients who must undergo regular evaluations. The non-invasive nature of the scan means that patients can avoid the discomfort and anxiety often associated with more intrusive methods like bone marrow biopsies. This is especially crucial for a disease that impacts approximately 33,000 individuals in the UK, with thousands of new diagnoses each year. The ability to conduct frequent assessments without compromising patient well-being fosters a more sustainable approach to disease monitoring. Moreover, the comfort provided by this technology can enhance patient compliance with follow-up care, ensuring that clinicians receive consistent data to guide treatment decisions. As healthcare systems strive to balance efficacy with empathy, whole-body MRI emerges as a beacon of progress in creating diagnostic solutions that respect both medical needs and human experience.
Human Impact Through Personal Resilience
The transformative potential of whole-body MRI becomes profoundly evident through the lived experience of individuals like Fin Monahan, a South Wales firefighter and former RAF officer who has battled myeloma since his diagnosis over a decade ago. Having endured two relapses, Monahan’s journey took a significant turn for the better when this advanced imaging technology detected early signs of cancer recurrence that traditional tests missed. This timely identification enabled swift intervention, extending his life and preserving his ability to engage in demanding professional roles, from piloting jets to leading high-stakes operations abroad. His story serves as a powerful testament to how cutting-edge diagnostics can offer not just medical benefits but also the chance to maintain a semblance of normalcy amidst a chronic illness, highlighting the profound personal impact of such innovations.
Expanding on this narrative, Monahan’s experience underscores the broader implications of whole-body MRI for quality of life among myeloma patients. The early detection facilitated by this technology did more than just alter his treatment timeline; it provided a psychological lifeline by reducing the uncertainty that often accompanies cancer relapses. Knowing that even the smallest traces of disease could be identified and addressed offered reassurance during a mentally taxing battle. Beyond individual resilience, his ability to continue contributing to society in high-pressure roles illustrates how advanced diagnostics can ripple outward, benefiting communities and organizations as well. This personal account reinforces the idea that medical advancements are not merely technical achievements but also tools that empower patients to reclaim agency over their lives, bridging the gap between clinical outcomes and human aspirations.
Pioneering the Future of Oncology
Experts in the field, including Professor Christina Messiou and Professor Martin Kaiser, have hailed whole-body MRI as a “gold standard” in precision imaging, recognizing its critical role in advancing personalized cancer care. By delivering detailed insights into the distribution of disease and individual responses to therapy, this technology enables clinicians to craft treatment plans tailored to each patient’s unique profile. Its integration into clinical practice at The Royal Marsden Hospital exemplifies a forward-thinking approach, signaling a shift toward embedding state-of-the-art imaging in routine care. As oncology increasingly embraces precision medicine, whole-body MRI stands at the forefront, offering a blueprint for how diagnostics can evolve to meet the complex demands of modern treatment paradigms, ultimately aiming for better survival rates and enhanced patient experiences.
Looking ahead, the widespread adoption of whole-body MRI holds immense promise for reshaping cancer care on a global scale. The technology’s ability to provide actionable data is becoming ever more vital as new therapeutic options for myeloma emerge, necessitating tools that can accurately assess their impact. Its non-invasive nature further supports its scalability, making it feasible for broader implementation across diverse healthcare settings. As research continues to validate its efficacy, there is growing momentum to establish this method as a standard in diagnostic protocols, potentially benefiting countless patients worldwide. The journey of whole-body MRI reflects a larger trend toward smarter, kinder medical solutions, where the focus is not only on curing disease but also on improving how patients navigate their health challenges, setting a precedent for innovation in oncology.