The invisible wounds of trauma have long presented a formidable challenge for modern medicine, particularly in the diagnosis of Post-Traumatic Stress Disorder, a condition historically reliant on the subjective and often fluctuating self-reports of patients. For the approximately 23% of 9/11 World Trade Center responders living with PTSD, this diagnostic ambiguity can create significant barriers to receiving timely and effective care. The absence of a definitive, objective biological marker has left clinicians without the concrete diagnostic tools available for many other medical conditions, forcing them to navigate a complex landscape of symptoms that can overlap with other mental health issues. This reliance on subjective inventories means that diagnosis can be influenced by a person’s willingness to disclose their experiences or their ability to articulate their internal state at a specific moment. A groundbreaking brain imaging study focused on these very responders has now provided compelling evidence that could revolutionize this landscape, revealing measurable, physical changes in the brain that correlate directly with a PTSD diagnosis, paving the way for a new era of objective mental health assessment.
Uncovering the Biological Footprint of Trauma
Advanced Imaging Techniques Unveil Brain Alterations
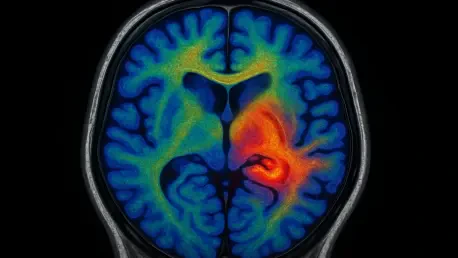
In a landmark investigation detailed in Biological Psychiatry: Cognitive Neuroscience and Neuroimaging, researchers analyzed the brains of 99 World Trade Center responders, roughly half of whom had been diagnosed with chronic PTSD. To peer into the microstructural integrity of their brains, the scientific team employed a highly specialized MRI-based technique known as gray-white contrast (GWC) neuroimaging. This sophisticated method goes beyond simply measuring the size or activity of brain regions; instead, it assesses the sharpness and distinctness of the boundary separating the brain’s gray matter from its white matter. In a healthy brain, this boundary is crisp and well-defined, reflecting an orderly and efficient architecture. Gray matter, dense with neuronal cell bodies, is primarily responsible for information processing, while white matter, composed of myelinated nerve fibers, acts as the brain’s communication network, transmitting signals between different regions. A clear demarcation between these two types of tissue is crucial for optimal neural function and signaling speed.
The selection of gray-white contrast neuroimaging was pivotal, as it provides a unique window into the brain’s fundamental structure that other common imaging modalities might miss. Unlike functional MRI (fMRI), which measures blood flow to infer brain activity, or standard structural MRI, which assesses the volume of different brain areas, GWC analysis offers a direct measure of tissue integrity at a microscopic level. A blurry or indistinct border, as identified by GWC, suggests a pathological change in the composition of the tissue itself, indicating that the normal architectural separation has been compromised. This approach allowed researchers to detect subtle but widespread abnormalities that are not about a brain region shrinking or becoming overactive, but about the very nature of the tissue changing. This level of detail is critical because it moves the focus from macroscopic changes to the underlying cellular and structural health of the brain, offering a more fundamental understanding of how severe trauma can physically reshape the organ responsible for our thoughts, emotions, and memories.
The Blurring Lines of Neural Matter
The study’s central and most startling discovery was a significant and widespread reduction in the distinctness of the gray-white matter boundary among the responders with chronic PTSD. This low GWC value indicates that the gray matter in these individuals had taken on characteristics more typical of white matter. The researchers theorize that this blurring is caused by an abnormal concentration of myelin—the fatty, insulating sheath that normally envelops the axons of white matter—infiltrating the gray matter regions. This structural anomaly suggests a profound disruption in the brain’s organization, potentially impairing its processing speed and consistency. The integrity of the gray-white matter boundary is essential for efficient neuronal signaling, and its compromise could explain many of the cognitive and emotional difficulties experienced by those with PTSD. The fact that these changes were not confined to a single, isolated brain region but were observed across the cortex underscores the pervasive and systemic impact of severe trauma on the brain’s physical architecture.
Further analysis revealed a powerful and specific link between the degree of boundary blurring and the severity of a particular cluster of PTSD symptoms: re-experiencing. This category includes the disorder’s most hallmark and intrusive symptoms, such as debilitating flashbacks, nightmares, and involuntary, distressing memories of the traumatic event. The strong correlation suggests that the observed physical changes in the brain’s structure are not just a general marker of the disorder but may be directly tied to the neural mechanisms that cause traumatic memories to be replayed against a person’s will. This finding is exceptionally important because it provides a tangible, biological explanation for one of the most painful and disorienting aspects of living with PTSD. By connecting a specific, measurable brain abnormality to a core subjective experience, the research strengthens the argument that PTSD is a neurological injury, not just a psychological reaction, and provides a clear target for future research into treatments that could potentially reverse or mitigate these structural changes.
From Subjective Reports to Objective Diagnosis
Pioneering Objective Biomarkers for PTSD
The profound implications of these findings extend far beyond the laboratory, establishing a firm biological foundation for a condition often misunderstood. For years, the lack of physical evidence has contributed to the stigmatization of PTSD, but this research demonstrates that severe trauma can physically reshape the brain’s neural integrity. The observed cortical differences in gray-white matter contrast present a promising candidate for an objective surrogate biomarker. Researchers propose that GWC analysis could be integrated into the diagnostic process, supplementing existing symptom-based inventories and clinical interviews. By combining this objective neuroimaging data with subjective patient reports, clinicians could achieve a more comprehensive and accurate assessment. This dual approach would allow for a more confident differentiation between trauma-exposed individuals who have developed PTSD and those who have not, reducing the reliance on a person’s state of mind at a single point in time and providing a more stable, biological anchor for diagnosis. This marks a critical move toward aligning the diagnosis of mental health disorders with other fields of medicine.
The development of an objective biomarker carries significant potential for enhancing early screening and preventative strategies, especially for high-risk populations. First responders, active-duty military personnel, and veterans are routinely exposed to traumatic events, yet identifying who among them will develop chronic PTSD has remained a persistent challenge. With a tool like GWC imaging, it may become possible to screen individuals soon after a traumatic event to detect the initial signs of these structural brain changes, potentially even before the full spectrum of psychological symptoms has manifested. Such early detection could trigger proactive interventions, such as targeted therapies or pharmacological treatments designed to halt or reverse the pathological process. This represents a paradigm shift from the current model of reactive care—waiting for a disorder to become entrenched before starting treatment—to one of proactive mental health management. By identifying at-risk individuals based on biological evidence, a window of opportunity could open for interventions that prevent the transition from acute stress to a chronic, debilitating condition.
A New Horizon in Mental Health Care
This landmark investigation represented a crucial turning point in the long and arduous quest for a biological understanding of post-traumatic stress. The study not only provided some of the most compelling evidence to date that the invisible wounds of trauma have a physical, measurable signature in the brain but also offered a tangible path forward. For the first time, the prospect of an objective, biological test for PTSD moved from a distant scientific aspiration to a concrete possibility. The identification of blurred gray-white matter boundaries as a potential biomarker gave researchers a specific and promising target for future inquiry and clinical tool development. This work laid the groundwork for subsequent studies aimed at refining these imaging techniques and exploring whether these brain changes could be reversed with effective treatment. The hope it offered to countless individuals, particularly the WTC responders who participated, was that their suffering could be validated not just by their words, but by objective science, ultimately leading to more precise diagnostics and innovative therapies for a condition that had remained in the shadows for far too long.