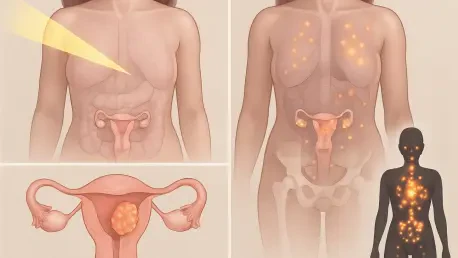
Endometrial cancer, recognized as the most prevalent gynecologic malignancy across the globe, continues to present a formidable challenge to healthcare systems with its steadily increasing incidence and mortality rates, impacting countless lives each year. For patients diagnosed at an early stage, surgical interventions such as hysterectomy often provide a viable path to recovery. However, the outlook for those with advanced, recurrent, or disseminated disease remains bleak due to the scarcity of effective targeted therapies. This critical gap in treatment options has fueled urgent research into innovative approaches, with a recent study published in The Journal of Nuclear Medicine unveiling a significant breakthrough. Spearheaded by Brian M. Zeglis, PhD, alongside a collaborative team from Hunter College and Memorial Sloan Kettering Cancer Center, the research delves into novel molecular targets that could revolutionize both the diagnosis and treatment of this pervasive disease. The promise of these findings lies in their potential to offer hope where current medical strategies fall short.
The concept of radiotheranostics, a pioneering method that integrates diagnostic imaging with targeted therapeutic delivery through radioactive agents, stands at the heart of this research. By focusing on molecular markers unique to endometrial cancer, scientists aim to enhance the precision of tumor detection while simultaneously administering treatments tailored to individual patients. Such an approach could dramatically improve outcomes, particularly for those who currently face limited options under existing clinical protocols. The study’s emphasis on combining these dual capabilities underscores a transformative shift in managing a disease that disproportionately affects women worldwide, setting the stage for a deeper exploration of its methodologies and implications.
Advancements in Precision Medicine for Endometrial Cancer
Unlocking Potential with Molecular Biomarkers
The recent research places significant emphasis on three molecular biomarkers—human epidermal growth factor receptor 2 (HER2), mucin-16 (MUC16), and cluster of differentiation 24 (CD24)—as prospective targets for radiotheranostic applications. Through the use of positron emission tomography (PET) imaging, specialized probes were developed and tested in preclinical models to visualize these biomarkers effectively. The findings revealed that HER2 and CD24 exhibited notably high expression levels in cancerous tissues compared to healthy endometrial samples, positioning them as prime candidates for further exploration. This differential expression offers a critical opportunity to distinguish malignant cells non-invasively, paving the way for more accurate diagnostic tools that could redefine early detection strategies in clinical settings. The ability to pinpoint these markers with such clarity suggests a future where diagnosis is not just a starting point but a tailored guide to therapy.
Moreover, the standout performance of the CD24-targeted probe in preclinical testing adds a layer of optimism to these developments. Demonstrating exceptional tumor uptake and superior imaging contrast, this probe outperformed its counterparts, indicating strong potential for both identifying tumors and possibly delivering targeted radiation therapy. In comparison, the HER2 probe showed promising yet moderate results, hinting at its applicability for a specific subset of patients with overexpressed HER2 in their tumors. Meanwhile, the MUC16 probe did not achieve the same level of efficacy, highlighting the nuanced challenges in developing universally effective radiotheranostic agents. These varied outcomes emphasize the importance of continued research to refine these tools, ensuring they meet the diverse needs of patients grappling with this malignancy.
Transforming Clinical Approaches
The implications of these radiotheranostic advancements extend far beyond mere detection, offering a transformative approach to the clinical management of endometrial cancer. By leveraging PET imaging to identify patients with elevated HER2 or CD24 expression, healthcare providers could craft personalized treatment plans that maximize therapeutic impact while minimizing unnecessary side effects. This precision-driven strategy addresses a longstanding issue in cancer care where one-size-fits-all treatments often fail to account for individual biological differences. The potential to tailor interventions based on specific biomarker profiles marks a significant departure from traditional methods, promising improved survival rates for those with advanced or recurrent disease who currently face limited options.
Additionally, the dual functionality of radiotheranostic agents—combining diagnostic visualization with targeted radiation delivery—holds the power to redefine therapeutic standards. This approach allows for precise attacks on cancer cells while sparing surrounding healthy tissues, reducing the collateral damage often associated with conventional radiation therapies. Such innovation is particularly crucial for a disease like endometrial cancer, which has historically received less attention in nuclear medicine compared to other malignancies such as breast or prostate cancer. By bringing this understudied area into focus, the research not only addresses immediate clinical needs but also sets a precedent for integrating cutting-edge technology into routine care, potentially altering the trajectory of patient outcomes on a broader scale.
Future Pathways and Broader Significance
Transitioning from Lab to Patient Care
Looking toward the horizon, the research team strongly advocates for the initiation of clinical trials to assess the safety and efficacy of HER2- and CD24-targeted radiotheranostic agents in human subjects. Transitioning from preclinical success to real-world application represents the next critical phase in validating these promising findings. The robust performance of these probes in murine models and patient-derived xenografts provides a compelling foundation, yet human trials are essential to uncover any unforeseen challenges or side effects. This step is pivotal in ensuring that the benefits observed in controlled environments translate effectively into tangible improvements for patients battling endometrial cancer, bridging the gap between laboratory innovation and bedside care.
Furthermore, the study suggests exploring combination therapies that target multiple molecular markers simultaneously to address the inherent heterogeneity of endometrial tumors. Given that cancer often presents with diverse biological characteristics within a single patient, relying on a singular target may not suffice for comprehensive treatment. Investigating synergistic approaches could enhance therapeutic outcomes by tackling various aspects of tumor biology concurrently. This forward-thinking strategy underscores the necessity of adaptability in medical research, encouraging the development of multifaceted solutions that can evolve alongside the complexities of the disease. Such efforts are poised to refine the precision of radiotheranostics, ensuring they meet the nuanced demands of clinical practice over the coming years.
Catalyzing Focus on an Overlooked Malignancy
The broader impact of this groundbreaking work lies in its capacity to elevate endometrial cancer within the nuclear medicine community, spotlighting a malignancy that has often been overshadowed by more extensively studied cancers. By demonstrating the tangible potential of radiotheranostic approaches, the study could inspire increased funding and research interest, driving innovation in an area long in need of attention. This shift is crucial, as heightened focus may accelerate the development of novel diagnostic and therapeutic tools, ultimately benefiting countless patients who currently face limited options. The momentum generated by these findings has the power to reshape priorities within oncology, ensuring that resources are allocated to address disparities in research focus.
Equally significant is the potential for this research to catalyze a paradigm shift from generic treatment protocols to highly personalized, precision-based care. The successful identification of HER2 and CD24 as viable targets through PET imaging reflects a broader trend toward tailoring medical interventions to individual patient profiles. This evolution in approach not only promises better outcomes for those affected by endometrial cancer but also sets a model for other understudied diseases to follow. As the field of nuclear medicine continues to embrace such targeted strategies, the legacy of this study may well be its role in fostering a more equitable landscape of cancer care, where every patient benefits from advancements tailored to their unique needs.