I’m thrilled to sit down with Ivan Kairatov, a distinguished biopharma expert with a wealth of experience in research and development, particularly in the intersection of technology and innovation in healthcare. Today, we’re diving into a groundbreaking advancement in the field of neurosurgery: a new nomogram designed to predict long-term survival in patients with brain abscesses. Our conversation will explore the seriousness of this condition, the inspiration behind this innovative tool, the key findings from the research conducted in southern Thailand, and how this dynamic nomogram could transform clinical decision-making for better patient outcomes.
Can you start by explaining what a brain abscess is and why it remains such a critical health issue?
A brain abscess is a localized infection within the brain tissue, often occurring in the parenchyma, which is the functional part of the brain responsible for critical processes. It’s a severe condition because it can cause swelling, inflammation, and pressure on surrounding brain structures, potentially leading to neurological damage. Despite advancements in medical and surgical treatments, it still frequently results in disability or death due to delayed diagnosis, the complexity of treating infections in such a sensitive area, and the risk of complications like brain swelling or rupture of the abscess.
What motivated you to delve into predicting long-term survival for brain abscess patients?
The motivation came from a clear gap in our understanding of how to predict outcomes over extended periods for these patients. While we’ve identified some short-term prognostic factors, long-term survival remained a gray area. I wanted to provide clinicians with tools to make more informed decisions and help patients and families understand what to expect. Focusing on southern Thailand for this study was a strategic choice due to the high incidence of cases in that region and access to a tertiary care hospital with comprehensive patient data, which allowed for a robust retrospective analysis.
Can you walk us through the most significant findings from your research?
Certainly. Our study, which analyzed data from 205 patients, pinpointed several key predictors of long-term survival. These include age, overall health status as measured by the Karnofsky performance scale, blood culture results, preoperative blood clotting issues, specific blood cell ratios like neutrophil-to-lymphocyte, the presence of immature white blood cells, and even the location of the abscess—particularly in the occipital region. These factors collectively paint a picture of how the body’s response and the abscess’s position in the brain influence recovery and survival over time.
You’ve highlighted specific survival probabilities over different time frames. Can you elaborate on what these numbers mean?
Absolutely. We found that the survival probabilities for brain abscess patients were 77% at one year, 73% at two years, and 69% at five years. These figures indicate that while many patients survive the initial crisis, there’s a gradual decline over time, reflecting the lingering impact of the condition or related complications. Compared to historical data, where mortality rates ranged widely from 10% to 40%, our 5-year survival rate of 69% suggests we’re making progress, but the fatality rate is still significant, underscoring the need for better prognostic tools and interventions.
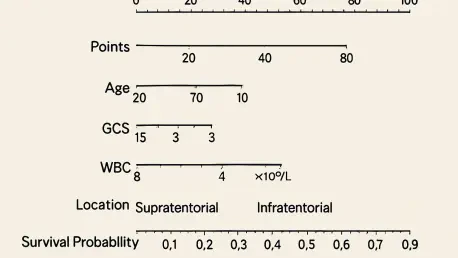
Let’s talk about the nomogram you developed. Can you explain what it is and how it functions?
A nomogram is essentially a graphical tool that allows clinicians to input specific patient data and get a personalized prediction of outcomes—in this case, long-term survival for brain abscess patients. We opted for a dynamic nomogram, which is interactive and web-based, over a static chart because it can adapt to real-time inputs and provide more precise estimations. Doctors can enter variables like age, lab results, and abscess location, and the tool calculates a survival probability, helping guide treatment plans and patient counseling.
How confident are you in the reliability of this nomogram based on your validation results?
We’re quite confident in its performance. The nomogram showed a strong predictive ability with a C-index of 0.855 in initial validation and 0.701 in testing data, which are solid indicators of accuracy in statistical models. Additionally, calibration plots and other analyses confirmed that the predicted outcomes closely matched actual results. These validations suggest the tool isn’t just theoretically sound but practically reliable for clinical use, though we still advocate for ongoing refinement and external testing.
How do you envision this nomogram being integrated into everyday clinical practice?
I see it becoming a go-to resource for neurosurgeons and infectious disease specialists when managing brain abscess cases. It can inform critical decisions, like whether to pursue aggressive surgical intervention or tailor rehabilitation plans based on predicted outcomes. It’s particularly useful for patients with complex profiles—those with multiple risk factors or unusual abscess locations—where standard protocols might not fully apply. Ultimately, it empowers clinicians to personalize care and improve communication with patients about their prognosis.
What challenges or limitations did you encounter while conducting this research?
Gathering detailed, consistent data from a retrospective cohort of 205 patients was no small feat. There were instances of incomplete medical records or variations in how data was documented over the study period from 2014 to 2024. Additionally, since our research was based in a specific region, there’s a question of how generalizable the findings are to other populations with different healthcare systems or infection patterns. These limitations highlight the need for broader studies to validate and adapt our model further.
Looking ahead, what is your forecast for the future of brain abscess treatment and prognostication?
I’m optimistic that we’re on the cusp of a new era in managing brain abscesses. With tools like dynamic nomograms, we’re moving toward precision medicine, where treatments and predictions are tailored to the individual. I foresee further integration of technology—think artificial intelligence and machine learning—enhancing these models with even greater accuracy. Additionally, as we expand research to diverse populations and refine our understanding of infection mechanisms, I believe we’ll see improved therapies and lower mortality rates over the next decade, making this condition far less devastating.