The ongoing battle against highly aggressive blood cancers has reached a pivotal moment with the emergence of a groundbreaking therapy that demonstrated remarkable effectiveness in recent clinical trials. Comprehensive data presented at the 67th American Society of Hematology (ASH) Annual Meeting unveiled significant therapeutic potential for pivekimab sunirine (PVEK), a novel antibody-drug conjugate (ADC), in treating both acute myeloid leukemia (AML) and blastic plasmacytoid dendritic cell neoplasm (BPDCN). Research spearheaded by investigators at The University of Texas MD Anderson Cancer Center positions this innovative agent, which targets the CD123 antigen, as a promising new weapon for patients who have long faced grim prognoses and limited curative options. This development not only offers renewed hope but also underscores a critical shift in hematology toward precision-targeted therapies capable of delivering enhanced efficacy with a more manageable toxicity profile.
Mechanism and Validation of a Key Target
A Precision-Guided Weapon Against Cancer
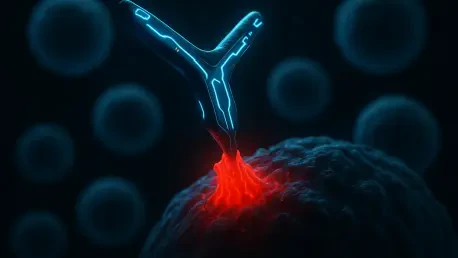
Pivekimab sunirine represents a sophisticated evolution in cancer therapy, functioning as a highly targeted delivery system for a potent cell-killing agent. Unlike traditional antibody treatments that primarily work by recruiting the patient’s own immune system, PVEK is engineered for direct cytotoxic impact on malignant cells. Its mechanism hinges on its ability to selectively bind to the CD123 protein, an antigen that is frequently overexpressed on the surface of AML cells and is a universal marker in BPDCN. Once the ADC latches onto this target, the cancer cell internalizes it. Inside the cell, PVEK releases its formidable payload: an indolinobenzodiazepine pseudodimer. This potent agent is designed to induce fatal DNA strand breaks. A key feature of its design is that it achieves this without crosslinking DNA, a mechanism intended to maximize the destruction of cancer cells while potentially offering a distinct and more tolerable toxicity profile compared to the harsh effects of many conventional chemotherapies.
The strategic design of this antibody-drug conjugate provides a significant advantage in modern oncology, particularly in the context of treatment resistance. The direct-delivery system is engineered to maintain its powerful activity even in diseases that have developed mechanisms to evade standard cytotoxic drugs, which often rely on different cellular pathways. By bypassing these common resistance pathways, pivekimab sunirine offers a new line of attack. This precision is crucial, as it concentrates the therapy’s destructive power where it is needed most—inside the malignant cells—thereby minimizing collateral damage to healthy tissues. This targeted approach is fundamental to the ADC platform’s promise: to achieve deeper and more durable remissions without proportionally increasing the treatment burden on the patient. The success of PVEK in early trials validates this principle, showing that a well-designed ADC can effectively thread the needle between potent efficacy and manageable safety.
Validating the CD123 Target
For many years, the scientific community has recognized the CD123 antigen as a compelling and theoretically ideal target in the fight against various hematologic cancers. Its high level of expression on malignant cells, coupled with lower expression on essential healthy hematopoietic stem cells, made it an attractive candidate for targeted therapies. However, translating this theoretical promise into a clinically effective treatment proved to be a formidable challenge. Previous therapeutic strategies aimed at CD123, which included immunotoxins and unconjugated antibodies, were frequently hampered by significant limitations. These earlier attempts often struggled to achieve the necessary potency to eliminate the cancer cells effectively or were associated with severe off-tumor side effects that made them too toxic for widespread clinical use. This history of setbacks left a critical unmet need and underscored the difficulty of successfully leveraging this otherwise perfect target for patient benefit.
The recent clinical data presented for pivekimab sunirine signifies a watershed moment, suggesting that its optimized and intelligent design has finally surmounted these long-standing historical obstacles. The cohesive narrative emerging from the AML and BPDCN trials strongly supports the idea that PVEK has succeeded where its predecessors fell short. This success can be attributed to the sophisticated engineering of the ADC, which combines a highly specific targeting antibody with a potent and well-characterized payload. This combination ensures that the therapy is delivered with precision and unleashes its cytotoxic effect primarily within the cancer cells. By doing so, PVEK not only demonstrates remarkable clinical activity but also validates CD123 as a critical and druggable therapeutic target. This achievement represents a significant advancement, breathing new life into a promising area of research and affirming the power of the ADC platform to turn biological insights into tangible clinical breakthroughs for patients.
Clinical Breakthroughs in Two Cancers
Transforming Treatment for Acute Myeloid Leukemia (AML)
A key highlight from the recent data involved a Phase Ib/II clinical trial that investigated pivekimab sunirine as part of an innovative triplet combination therapy. The study focused on a particularly challenging patient demographic: newly diagnosed older adults with AML who are deemed ineligible for the rigors of intensive induction chemotherapy. For this population, the combination of venetoclax and azacitidine has become a vital standard of care, yet treatment failures and the inevitable emergence of resistance remain significant clinical hurdles. The trial was designed to explore whether adding PVEK to this established dual-agent regimen could deepen patient responses and improve outcomes without introducing prohibitive new side effects. The results from the 49 patients treated were exceptionally encouraging, demonstrating impressive remission rates that surpassed expectations. Specifically, over 63% of patients achieved a complete remission, while nearly 80% reached a composite endpoint of complete remission with or without the incomplete recovery of blood counts.
The significance of these findings extends beyond the high initial response rates, pointing toward the potential for more durable disease control. A critical indicator of long-term success, measurable residual disease (MRD) negativity, was achieved in the majority of patients who responded to the triplet therapy, suggesting a profound level of disease clearance at the molecular level. This deep remission is often a prerequisite for lasting cures. Furthermore, the therapy’s success was validated by the fact that several patients were able to proceed to an allogeneic stem cell transplantation—a potentially curative procedure that is frequently inaccessible to this patient group due to persistent disease or an inability to tolerate pre-transplant conditioning. Importantly, the addition of PVEK to the standard regimen did not introduce any new or unexpected safety concerns. This outcome supports the compelling hypothesis that strategically replacing, rather than simply intensifying, cytotoxicity with a targeted agent can lead to deeper and more meaningful remissions without a corresponding increase in risk to the patient.
A New Standard for Blastic Plasmacytoid Dendritic Cell Neoplasm (BPDCN)
The second major area of focus was the Phase I/II CADENZA study, which evaluated pivekimab sunirine as a monotherapy for treating blastic plasmacytoid dendritic cell neoplasm. This rare and highly aggressive malignancy represents an ideal candidate for a CD123-targeted therapy because the antigen is uniformly and strongly expressed across virtually all documented cases, providing a consistent and reliable target for the drug. The presentation at the ASH meeting, led by Dr. Naveen Pemmaraju, provided a detailed analysis of a particularly vulnerable and historically poor-prognosis subgroup: BPDCN patients who also have prior or concomitant hematologic malignancies (PCHM), such as myelodysplastic syndromes or chronic myelomonocytic leukemia. This subgroup, which constituted approximately one-third of the frontline patient cohort, typically fares much worse due to complicating factors like compromised bone marrow function and narrower therapeutic windows for treatment.
Despite these unfavorable baseline characteristics and a median patient age of 73, PVEK monotherapy demonstrated remarkable and unprecedented efficacy. The overall response rate within this high-risk PCHM subgroup reached an impressive 90.9%, with a composite complete response rate of 63.6%, indicating that the majority of these patients achieved a deep clinical remission. The median overall survival was 17 months, an outcome that the investigators noted either rivals or surpasses the historical benchmarks for this devastating disease, even in healthier patient populations. Underscoring both the treatment’s profound effectiveness and its notable tolerability, nearly half of the patients in this challenging subgroup were successfully bridged to a potentially curative stem cell transplant. This finding is particularly noteworthy as it highlights PVEK’s robust single-agent activity, which is driven by the strong biological rationale of precisely targeting a universally expressed antigen on the cancer cells.
The Path Forward From Trial to Clinic
While the initial clinical results were highly encouraging, the journey to bring pivekimab sunirine to patients required critical subsequent steps. Longer-term follow-up from both the AML and BPDCN trials was essential to confirm that the high initial response rates translated into durable disease control and, ultimately, improved overall survival for patients. For the AML indication, the promising outcomes from the triplet therapy necessitated confirmation in a larger, randomized controlled trial to definitively establish its superiority over the existing venetoclax-azacitidine standard of care. For BPDCN, the rarity of the disease presented unique challenges for conducting large comparative trials, but the exceptional strength of the CADENZA results provided a compelling rationale for pursuing a registrational pathway. In review, the clinical data for pivekimab sunirine presented at the ASH meeting marked a significant and tangible advancement, offering genuine hope and outlining a potential new treatment paradigm for patients with AML and BPDCN who had previously faced grim prognoses and severely limited therapeutic options.