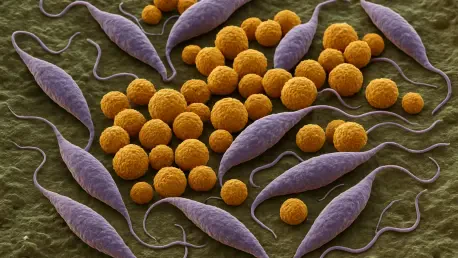
Leishmaniasis, a debilitating infectious disease caused by the protozoan parasite Leishmania, continues to afflict millions of people worldwide, predominantly in under-resourced regions where access to effective healthcare remains a significant challenge. Among its numerous species, Leishmania amazonensis is particularly notorious for its severe impact on public health, causing disfiguring lesions and systemic complications. Traditional treatments, such as amphotericin B, have long been a cornerstone in combating this parasite, yet they come with significant drawbacks, including systemic toxicity, kidney damage, and high costs that burden vulnerable populations. A pioneering study published in Scientific Reports this year unveils a revolutionary approach using alternating magnetic field (AMF)-responsive nanobiomagnetite particles to deliver amphotericin B directly to infection sites. This innovative system promises to enhance treatment efficacy while drastically reducing side effects, offering a glimmer of hope for those grappling with this devastating disease in endemic areas.
Harnessing Nanotechnology for Precision Medicine
The advent of nanotechnology has opened new frontiers in medical treatment, and this latest research exemplifies its potential to transform the management of parasitic infections like leishmaniasis. The AMF-responsive nanobiomagnetite system is designed to act as a smart delivery mechanism for amphotericin B, utilizing magnetic fields to guide tiny nanoparticles directly to the areas of the body infected by Leishmania amazonensis. This targeted approach ensures that the drug is concentrated where it is most needed, rather than circulating broadly through the bloodstream, which often leads to unnecessary toxicity in healthy tissues. By focusing the therapeutic effect, the system reduces the overall dosage required, thereby minimizing the risk of severe side effects that have long plagued conventional treatments. Such precision not only boosts the drug’s effectiveness but also represents a significant step toward safer medical interventions for complex diseases.
Safety remains a critical consideration in the development of this technology, and the research team has prioritized biocompatibility in the design of the nanobiomagnetite particles. Crafted from materials that pose minimal risk to the human body, these nanoparticles are engineered to protect amphotericin B from premature degradation, ensuring its stability during transit to the infection site. Furthermore, the system allows for controlled release of the drug, modulated by exposure to AMFs, which prevents sudden spikes in concentration that could harm patients. This careful balance of stability and controlled delivery underscores the potential of nanotechnology to address not only efficacy but also patient well-being, marking a notable advancement over traditional methods that often struggle with maintaining consistent therapeutic levels without adverse reactions.
Tackling the Socioeconomic Challenges of Leishmaniasis
Leishmaniasis imposes a profound socioeconomic burden, particularly in regions where Leishmania amazonensis is prevalent, often affecting communities with limited access to adequate healthcare infrastructure. The high cost of treatments like amphotericin B, coupled with the need for prolonged administration and monitoring due to toxicity risks, exacerbates the strain on both patients and local health systems. The introduction of the nanobiomagnetite delivery system offers a promising solution by potentially lowering the required drug dosage and reducing treatment duration, which could translate into more affordable care. By addressing these economic barriers, the technology aligns with global health initiatives aimed at improving equity and ensuring that effective treatments reach those who need them most, regardless of financial constraints.
Beyond cost considerations, the research also emphasizes the public health impact of leishmaniasis in endemic areas, where the disease contributes to cycles of poverty and disability due to its debilitating effects. The targeted delivery approach shows encouraging preliminary results against Leishmania amazonensis, suggesting that it could significantly improve patient outcomes and reduce the long-term consequences of infection. This focus on a specific species highlights the tailored nature of the solution, addressing the unique challenges posed by this parasite while paving the way for scalable interventions. If successful in broader clinical applications, this system could help break the cycle of hardship associated with leishmaniasis, offering not just medical relief but also a chance for affected communities to rebuild and thrive.
Boosting Treatment Through Immune Synergy
One of the more intriguing aspects of the nanobiomagnetite system lies in its potential to enhance the body’s natural defenses alongside direct drug delivery. By concentrating amphotericin B at the site of infection, the nanoparticles may inadvertently draw attention from the immune system to the affected area, possibly stimulating a stronger response against Leishmania amazonensis. This synergy between targeted therapy and immune activation could amplify the overall effectiveness of the treatment, providing a dual mechanism to combat the parasite. Such an approach marks a departure from traditional methods that rely solely on the drug’s direct action, hinting at a more integrated strategy for managing infectious diseases.
This potential immune-modulating effect also raises interesting possibilities for optimizing therapeutic outcomes beyond simply killing the parasite. If the system can indeed bolster the host’s immune response, it might reduce the likelihood of relapse or reinfection, a common challenge in leishmaniasis treatment. The research suggests that this added layer of defense could be particularly beneficial in regions where patients face repeated exposure to the parasite due to environmental factors. While further studies are needed to fully understand this interaction, the prospect of combining drug delivery with immune support underscores the innovative nature of the nanobiomagnetite platform, positioning it as a multifaceted tool in the fight against parasitic infections.
Exploring Future Horizons in Disease Management
While the primary focus of this research is on combating leishmaniasis, the implications of the AMF-responsive nanobiomagnetite system extend far beyond this single disease. The versatility of the technology suggests it could be adapted to address other vector-borne or parasitic conditions that similarly challenge global health efforts. In an era marked by rising drug resistance and the emergence of complex infectious threats, such adaptable solutions are increasingly critical. The ability to tailor the system for different pathogens highlights its potential as a cornerstone of future medical advancements, reflecting a broader trend toward personalized and precise therapies in biomedical science.
Looking ahead, the adaptability of this platform could inspire new research directions, encouraging scientists to explore its application in diverse therapeutic contexts. The integration of magnetic targeting with nanotechnology also sets a precedent for interdisciplinary collaboration, merging insights from materials science, pharmacology, and infectious disease management. As clinical trials and further studies progress, the system might evolve to tackle a wider array of health challenges, offering scalable and innovative answers to pressing medical needs. This forward-thinking approach not only addresses current limitations in leishmaniasis treatment but also lays the groundwork for a future where targeted therapies become the norm across various fields of medicine.
Reflecting on a Path Forward
In reflecting on this groundbreaking work, it becomes evident that the development of the AMF-responsive nanobiomagnetite system marks a pivotal moment in the battle against leishmaniasis. The research demonstrates remarkable potential in delivering amphotericin B with unprecedented precision to combat Leishmania amazonensis, significantly reducing the toxic side effects that once hindered treatment. The focus on biocompatibility and controlled release further ensures patient safety, while early results hint at enhanced efficacy that could transform lives in endemic regions. As a next step, expanding clinical trials to validate these findings on a larger scale emerges as a priority, alongside efforts to streamline production for cost-effectiveness. Additionally, exploring partnerships with global health organizations could accelerate the system’s deployment to those in dire need, ensuring that this innovation becomes a practical solution for millions. This journey of discovery underscores the power of nanotechnology to reshape medical care, pointing toward a hopeful horizon for managing infectious diseases worldwide.