Imagine a world where scientists can study the living human brain in real-time, unlocking secrets of neurological disorders without risking patient safety, a vision now closer to reality thanks to pioneering research from a leading medical institution. This study has tackled a longstanding challenge in neuroscience: safely obtaining brain tissue from living patients during deep brain stimulation (DBS) surgery, a procedure commonly used to manage conditions like Parkinson’s disease and depression.
Historically, neuroscience has relied heavily on post-mortem brain tissue for molecular and functional studies, as accessing live tissue posed significant risks. This limitation often meant that dynamic brain processes remained poorly understood, hindering progress in treatment development. The central question this research addresses is whether incorporating biopsies into DBS surgery heightens risks or negatively affects patient outcomes, a concern that has long deterred such approaches.
This investigation is significant because it challenges traditional barriers, potentially revolutionizing how brain research is conducted. By evaluating the safety of this method, the study paves the way for a deeper understanding of brain function and disease mechanisms, promising advancements that could benefit millions worldwide.
Background and Importance of the Research
DBS surgery stands as a cornerstone in treating severe neurological and psychiatric conditions, including Parkinson’s disease, obsessive-compulsive disorder, and treatment-resistant depression. During this elective procedure, electrodes are implanted into specific brain regions to modulate abnormal neural activity, offering relief where other therapies fail. Despite its clinical success, the procedure has not traditionally been leveraged for research purposes due to safety concerns.
A major limitation in neuroscience has been the dependence on post-mortem brain samples, which may not accurately reflect the active, living brain’s complexities. Such samples often fail to capture real-time cellular interactions or responses to disease, stunting the ability to develop targeted interventions. This gap has left researchers with an incomplete picture of how the brain operates under various conditions.
The importance of this study lies in its potential to bridge that gap by enabling access to living brain tissue during routine clinical procedures. This breakthrough could transform neuroscience, allowing for molecular studies and functional analyses that were previously impossible, thus enhancing the understanding of brain circuits and fostering innovative treatments.
Research Methodology, Findings, and Implications
Methodology
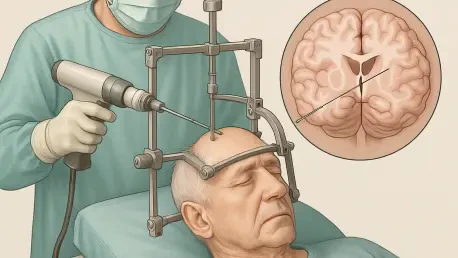
To assess the safety of prefrontal cortex biopsies during DBS surgery, a comprehensive retrospective analysis was conducted on a large cohort of patients. The study examined 1,152 DBS lead placements across 590 individuals at a single hospital over a span of more than a decade, starting from earlier records up to the present. These procedures were categorized into two groups: 652 with biopsies and 500 without, providing a robust comparison framework.
Biopsies were performed using a standardized punch tool to ensure precision and consistency in sample collection, targeting a small section of the prefrontal cortex before cauterization for electrode placement. Acute adverse events such as infections, intracranial hemorrhage, and seizures were meticulously tracked through medical records and post-operative CT scans for up to 90 days following surgery. Additionally, cognitive outcomes were evaluated over a one-year period in a subset of patients to gauge any long-term impact.
This rigorous methodology aimed to capture both immediate and delayed effects of the biopsy procedure, ensuring a thorough safety profile. The combination of detailed record-keeping and advanced imaging techniques provided a clear picture of potential risks associated with this innovative approach.
Findings
The results of this study are striking, demonstrating that prefrontal cortex biopsies during DBS surgery do not elevate the risk of complications compared to standard procedures. Notably, no infections were reported in either the biopsy or non-biopsy groups, alleviating a primary concern. Rates of intracranial hemorrhage were nearly identical, at 1.7% for the biopsy group and 1.4% for the non-biopsy group, with statistical insignificance (p=0.88).
Seizure occurrences also showed no meaningful difference, with rates of 0.2% in the biopsy group versus 0.4% in the non-biopsy group (p=0.82), further reinforcing the safety of the method. Moreover, cognitive assessments over one year revealed no significant decline linked to the number of biopsies taken, indicating that brain function remains unaffected by this additional step.
The consistency of biopsy sample sizes, with a mean volume of 40 cubic millimeters and a median of 30 cubic millimeters, highlights the reliability of the standardized technique. These findings collectively affirm that integrating biopsies into DBS surgery is a safe practice, opening new doors for research without compromising patient well-being.
Implications
The safety confirmation of this biopsy method marks a turning point for neuroscience, providing unprecedented access to living brain tissue for study. This capability can accelerate research into brain circuits, gene therapy applications, and the underlying mechanisms of complex disorders, potentially leading to novel therapeutic strategies.
Beyond immediate applications, the technique’s proven safety encourages its adoption across other medical centers, which could amplify the global impact of neuroscience research. Such widespread implementation might foster collaborative efforts, pooling data and insights to tackle pressing health challenges more effectively.
Furthermore, this study contributes to the push toward personalized medicine by integrating clinical observations with neuroimaging and molecular analyses. This holistic approach, as part of broader research initiatives, could tailor treatments to individual patients, enhancing outcomes for neuropsychiatric conditions and setting a new standard in medical practice.
Reflection and Future Directions
Reflection
This research exemplifies a remarkable balance between clinical care and scientific innovation, ensuring that patient safety remains paramount while pushing research boundaries. The collaboration with over 600 patients underscores the value of patient involvement in advancing medical knowledge, reflecting an ethical commitment to shared progress.
Challenges such as maintaining uniformity in biopsy techniques were addressed through meticulous standardization, minimizing variability and potential risks. This attention to detail was critical in establishing trust in the procedure’s safety and reliability across diverse surgical settings.
However, certain limitations, such as the focus on a single hospital’s data or the duration of follow-up, suggest areas for improvement. Expanding the study to include varied patient demographics or extending cognitive assessments over longer periods could provide an even fuller understanding of the method’s impact.
Future Directions
Looking ahead, further exploration of molecular insights derived from living brain tissue holds immense promise for unraveling the complexities of neuropsychiatric disorders. Detailed analyses could reveal new biomarkers or therapeutic targets, driving precision in diagnosis and treatment over the coming years.
Additionally, investigating the applicability of this biopsy technique in other neurosurgical contexts beyond DBS could broaden its utility. Adapting the method to different procedures might unlock further research opportunities, enhancing the scope of brain studies across various clinical scenarios.
Sustained investment and collaboration will be essential to assess long-term impacts and translate findings into therapeutic innovations. Encouraging multidisciplinary partnerships and funding initiatives starting from this year onward can ensure that the potential of this approach is fully realized, benefiting both science and patient care.
Concluding Insights on a Transformative Approach
This study concluded that prefrontal cortex biopsies during DBS surgery posed no increased risk of complications or cognitive decline, as evidenced by comparable adverse event rates between groups with and without biopsies. The meticulous data underscored the procedure’s reliability, setting a precedent for safely integrating research into clinical practice.
Moving forward, the medical and scientific communities should prioritize scaling this method across institutions to maximize its reach and impact. Establishing standardized protocols and training programs could facilitate adoption, ensuring consistency and safety worldwide.
Moreover, funding should be directed toward longitudinal studies to monitor outcomes over extended periods, potentially uncovering subtle effects or benefits not yet apparent. By fostering global cooperation and innovation, this breakthrough lays the groundwork for a new era in neuroscience, where real-time brain research could directly inform life-changing treatments.