The rare occurrence of primary intracranial immature teratomas in adults presents significant challenges for medical professionals. These tumors are exceedingly uncommon, particularly in adults, accounting for less than 1% of all primary intracranial malignancies. The rarity of such cases in females, especially involving the parietal lobe, highlights the uniqueness of these medical scenarios. Addressing this intricate case involves navigating complex diagnostic hurdles and carefully crafted treatment plans, with a thorough examination of literature being essential to understanding the current medical landscape regarding this condition.
Rare Occurrences in Adult Patients
Uncommon Demographic and Tumor Localization
Intracranial immature teratomas are predominantly found in children and young adults, often affecting males and typically located in midline structures such as the pineal gland and sellar region. Thus, the case of a 48-year-old woman presenting with a parietal lobe tumor signifies a notable deviation from the typical patient profile and location trends for this type of tumor. The patient’s age and gender contribute unique insight into the broader spectrum of demographic variations for these tumors. This case underscores the importance of considering atypical presentations and raises awareness among healthcare providers to remain vigilant even when presented with unusual patient demographics and tumor locations.
Analyzing Literature for Better Comprehension
A comprehensive review of the literature concerning intracranial immature teratomas underscores the rarity of such cases, especially among adult women. Historical analysis identifies only a limited number of documented cases involving adult females. These insights indicate a broader predominance of tumors in younger males, with frequent occurrence in midline brain structures rather than the parietal lobe. Examining previously reported cases deepens the understanding of variations in demographic and anatomical presentations, emphasizing the need for healthcare professionals to maintain heightened awareness of atypical manifestations. Such awareness is crucial in expanding diagnostic acumen and refining treatment approaches when managing rare tumor cases.
Navigating the Diagnostic Labyrinth
Distinguishing Teratomas from Gliomas
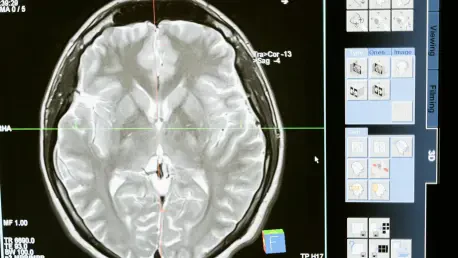
Diagnosing intracranial immature teratomas presents numerous challenges due to shared symptoms and imaging characteristics with other brain tumors, particularly gliomas. In this case, initial diagnostic imaging through computed tomography (CT) and magnetic resonance imaging (MRI) suggested a glioma diagnosis. Unique imaging features such as inhomogeneous density, mixed signal intensities, and associated perilesional edema contribute to frequent misdiagnosis. Relying solely on imaging may lead to diagnostic pitfalls if not complemented by a thorough histopathological examination, which was pivotal in this case for achieving an accurate diagnosis post-surgery. This diagnostic complexity spotlights the necessity for comprehensive evaluation methods that encompass advanced imaging techniques and detailed tissue analysis.
The Role of Histopathological Examination
This case exemplifies the critical role histopathology plays in confirming the suspected diagnosis. Despite imaging suggestive of glioma, histopathological analysis post-surgical resection revealed an intracranial immature teratoma. Such findings stress the imperative need for histopathology to complement imaging in ambiguous cases, as a definitive diagnosis validates treatment planning and execution. Histopathological involvement not only refines diagnostic precision but also informs therapeutic decision-making, ultimately aiding in the implementation of accurate and personalized management strategies for each patient.
Management and Treatment Considerations
Comprehensive Surgical Intervention
Surgical resection is highlighted as the cornerstone for treating primary intracranial immature teratomas. In this case, the patient underwent complete surgical removal of the tumor, followed by post-operative radiotherapy and regular monitoring. The initial successful outcome was tempered by tumor recurrence within eight months, necessitating a subsequent surgical intervention. This emphasis on surgical resection underscores its role as the primary treatment modality while also reflecting the unpredictability that often accompanies patient outcomes. Ongoing monitoring and readiness for potential re-intervention remain integral to patient care strategies, particularly given the potential for recurrence.
Evaluating Post-Operative Therapies
Post-surgical care for patients with intracranial immature teratomas often encompasses radiotherapy and, in certain scenarios, chemotherapy. However, therapeutic decisions must be meticulously weighed considering patient-specific factors, including age and overall health status, paralleling any recurrence risks or side effects. Balancing the benefits and risks of additional radiotherapy or chemotherapy entails personalized care tailored to each case’s nuances. Continuous follow-up and adaptation to evolving patient conditions are imperative, ensuring that the management aligns with patient needs and optimizes prognostic outcomes.
Illuminating Findings and Their Clinical Implications
Age and Gender Variability
The diversity in age and gender of patients with intracranial immature teratomas, as exemplified by this case, reinforces the importance of considering demographic variations during the diagnostic process. While prevalence skews toward young males, acknowledging and incorporating demographic deviations enriches clinical perspectives and aids in crafting more effective diagnostic hypotheses. Recognizing these findings broadens the understanding of the condition’s demographic profile and enables medical practitioners to foresee and adapt to different patient scenarios promptly.
Tumor Localization and Diagnostic Rigor
The parietal lobe location observed in this case serves as an unusual aspect to consider when diagnosing brain masses. Encouraging broader diagnostic inquiry when faced with atypical tumor locales can avert potential misdiagnosis and direct treatment effectively. The case underlines the necessity of a rigorous diagnostic process that surpasses imaging assumptions, advocating for thorough examinations that integrate histopathological analysis in uncertain conditions. These diagnostic enhancements lead to better-targeted interventions and significantly improve patient outcomes.
Consensus and Future Directions for Clinical Practice
Multidisciplinary Diagnostic and Treatment Approaches
Adopting a multidisciplinary approach proves essential for accurate diagnosis and effective treatment of rare intracranial tumors. This method involves integrating expertise from neurology, oncology, radiology, and pathology, creating a collaborative environment for evaluating and managing these complex medical scenarios. Such teamwork fosters comprehensive care pathways that address individual patient profiles while considering the evolving nature of a tumor’s behavior. Commitment to this collaborative strategy enhances clinical efficacy and ultimately refines treatment approaches.
Catalyzing Further Research and Discussion
The occurrence of primary intracranial immature teratomas in adults is exceptionally rare, posing significant challenges for medical professionals. These tumors are extremely uncommon, representing less than 1% of all primary intracranial malignancies. The unusual nature of such cases is even more pronounced in females, particularly when originating in the parietal lobe, which underscores the unique medical scenarios these conditions present. The management of this complex condition requires navigating intricate diagnostic hurdles and developing meticulously crafted treatment plans. A comprehensive examination of medical literature is essential to fully grasp the current landscape and advancement in understanding this condition. Since these tumors are so rare, especially in adults, specialists must rely on previous case studies and evolving research to derive the best approaches for diagnosis and treatment. Moreover, the rarity of these teratomas in females calls for heightened attention and a nuanced approach, ensuring every aspect of the case is considered. As these tumors may mimic other intracranial conditions, careful analysis and multiple diagnostic techniques must be employed to achieve accurate identification and effective intervention. The medical community’s ongoing study and documentation aim to improve outcomes and expand the knowledge base regarding intracranial immature teratomas in adults.