For decades, Body Mass Index (BMI) has served as the cornerstone for evaluating obesity-related health risks, guiding everything from clinical assessments to public health policies. Yet, a groundbreaking study from the University of Bristol’s Integrative Cancer Epidemiology Program (ICEP), published in the Journal of the National Cancer Institute, reveals that this widely used metric may not tell the full story. The research dives into the intricate relationship between body fat distribution and the risk of 12 obesity-related cancers, demonstrating that where fat accumulates—and the specific type of fat—matters just as much as, if not more than, overall body mass. This shift in perspective challenges the long-held reliance on a single number to predict health outcomes and raises compelling questions about how medical professionals assess and address cancer risk. By focusing on the nuances of fat storage, this study paves the way for a more individualized approach to prevention and treatment, urging a reevaluation of traditional health metrics in favor of deeper, more targeted insights.
The Shortcomings of Traditional Health Metrics
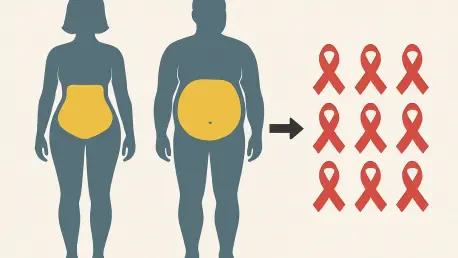
The simplicity of BMI has made it a popular tool for gauging health risks on a broad scale, but its limitations are becoming increasingly apparent. While it provides a quick snapshot based on height and weight, BMI fails to capture critical variations in how fat is distributed across the body. Two individuals with identical BMI scores might carry fat in entirely different areas—one around the abdomen, another in the hips and thighs—resulting in vastly different health implications. Lead researcher Emma Hazelwood, PhD, from the University of Bristol, argues that this oversight can obscure true cancer risks, leaving some patients misclassified as low-risk when they may face significant threats. The push to move beyond such a generalized metric is gaining traction in medical research, with experts advocating for assessments that account for individual differences in body composition to better predict disease outcomes.
This growing recognition of BMI’s inadequacy is not just academic—it has real-world consequences for patient care. Relying solely on this measure can delay the identification of at-risk individuals, particularly for cancers tied to specific fat deposits. For instance, abdominal fat might pose a greater threat for certain malignancies than overall weight suggests, while fat in other regions could play a neutral or even protective role. The ICEP study underscores the need for a paradigm shift, aligning with broader efforts in the health community to prioritize precision over simplicity. By integrating more detailed indicators into routine evaluations, clinicians could uncover hidden risks that BMI alone cannot reveal, ultimately enhancing the accuracy of cancer prevention strategies and ensuring that interventions are better tailored to each person’s unique profile.
Exploring the Diverse Impacts of Fat Types
Delving into the specifics, the ICEP research meticulously examines five distinct fat distribution traits—abdominal subcutaneous adipose tissue, visceral adipose tissue, gluteofemoral adipose tissue, liver fat, and pancreatic fat—and their connections to 12 specific cancers. The findings paint a complex picture: not all fat carries the same risk. For example, higher levels of visceral and liver fat are strongly associated with an elevated likelihood of liver cancer, while abdominal subcutaneous fat heightens risks for endometrial and esophageal adenocarcinoma. Conversely, gluteofemoral fat, often stored around the hips and thighs, appears to lower the chances of developing breast cancer and meningioma. This variability challenges the notion that obesity uniformly increases cancer risk and highlights the importance of looking at fat as a diverse, rather than monolithic, factor in health.
These revelations carry significant implications for how obesity-related cancers are understood and addressed. The protective effects of certain fat types, such as gluteofemoral adipose tissue, suggest that blanket weight-loss recommendations may not always be the best approach. Instead, focusing on reducing specific harmful fat deposits while preserving others could offer a more effective strategy for mitigating risk. The study’s granular approach to categorizing fat also emphasizes the need for advanced diagnostic tools that can accurately measure these distributions in clinical settings. As researchers continue to unravel the distinct roles of various fat types, the medical field must adapt by developing targeted interventions that account for these differences, moving away from one-dimensional solutions toward a more nuanced understanding of body composition and its impact on disease.
Cutting-Edge Approaches to Uncover Causality
A standout feature of the ICEP study is its innovative use of Mendelian randomization, a genetic epidemiology method that leverages inherited genetic variants to establish causal links between fat distribution and cancer risk. Unlike traditional observational studies, which often struggle with confounding variables and unreliable conclusions, this technique provides a more robust framework for determining cause and effect. By using genetic data as a proxy, the researchers were able to demonstrate with greater confidence that specific fat deposits directly influence the likelihood of developing certain cancers. This methodological advancement not only strengthens the study’s findings but also sets a new standard for investigating complex health relationships, offering a clearer path to actionable insights.
The adoption of such cutting-edge tools reflects a broader shift in medical research toward precision and reliability. Mendelian randomization helps overcome the limitations of past studies by minimizing bias and providing a firmer foundation for understanding how body fat impacts disease. This approach is particularly valuable in the context of personalized medicine, where establishing causality is crucial for designing effective interventions. As genetic research continues to evolve, it promises to refine the ability to predict individual risks with greater accuracy, potentially transforming how cancer prevention is approached. The success of this method in the ICEP study signals a promising direction for future investigations, encouraging the integration of genetic insights into mainstream health assessments to better inform clinical decision-making.
Decoding the Biological Pathways at Work
Beyond identifying associations, the ICEP research probes the underlying biological mechanisms that link fat distribution to cancer development, offering a deeper layer of understanding. Hormones and metabolic markers, such as bioavailable testosterone, fasting insulin, and adiponectin, emerge as key mediators in this relationship. For instance, the connection between abdominal subcutaneous fat and heightened endometrial cancer risk appears to be influenced by disruptions in sex hormone-binding globulin and testosterone levels. Meanwhile, the protective effect of gluteofemoral fat against certain cancers may be tied to elevated levels of adiponectin, a protein known for its anti-inflammatory properties. These findings shed light on the intricate ways in which fat interacts with the body’s systems to influence disease risk.
Unraveling these biological pathways is critical for translating research into practical solutions. Understanding why specific fat types contribute to or mitigate cancer risk opens the door to targeted therapies that address these mechanisms directly. For example, interventions could focus on modulating hormone levels or enhancing protective metabolic markers to reduce the impact of harmful fat deposits. This level of insight also underscores the need for interdisciplinary collaboration between geneticists, endocrinologists, and oncologists to fully explore these connections. As more studies build on these initial discoveries, the potential to develop innovative treatments that tackle the root causes of obesity-related cancers becomes increasingly tangible, promising a future where prevention is not just reactive but strategically informed by biology.
Redefining Cancer Prevention Strategies
The implications of the ICEP findings extend far into the realm of clinical practice, suggesting a fundamental rethinking of how cancer risk is assessed and managed. By incorporating fat distribution metrics into routine health evaluations, healthcare providers could more accurately identify individuals at heightened risk for specific cancers. For instance, patients with elevated visceral or liver fat might benefit from prioritized screening for liver cancer, while those with protective fat profiles could be guided toward different health focuses. This personalized approach stands in stark contrast to traditional methods that rely heavily on generalized BMI thresholds, offering a more precise toolset for early detection and prevention that aligns with each patient’s unique body composition.
Looking ahead, the research also hints at transformative possibilities for obesity treatment. Instead of aiming solely for overall weight reduction, strategies could be tailored to target harmful fat depots while preserving or even enhancing protective ones. This nuanced perspective could reshape dietary recommendations, exercise regimens, and even pharmacological interventions, ensuring they address the specific risks posed by fat distribution. Additionally, the call for prospective cohort studies to validate these findings reflects a commitment to building a robust evidence base that can inform policy and practice. As the medical community embraces these insights, the potential to improve patient outcomes through customized cancer prevention plans becomes a realistic and exciting prospect, marking a significant step forward in the fight against obesity-related diseases.