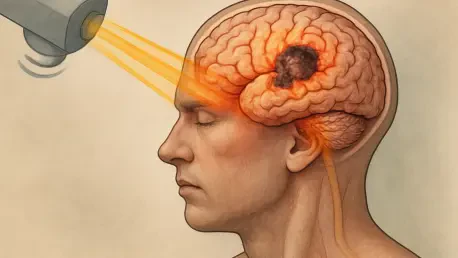
Diving into the complex world of radiation-induced brain injury (RIBI), we’re thrilled to speak with a leading expert in radiation oncology and neuroimaging. With years of experience in both clinical practice and cutting-edge research, our guest today has dedicated their career to understanding the challenges of RIBI and advancing diagnostic and therapeutic strategies. This conversation explores the underlying mechanisms of RIBI, its impact on patients, the role of innovative imaging techniques, and the future of targeted treatments, offering a glimpse into how science is moving toward precision care for this serious complication of cranial radiotherapy.
Can you explain in simple terms what radiation-induced brain injury, or RIBI, is for those who might not be familiar with it?
Absolutely. RIBI is a type of brain damage that can happen as a side effect of radiation therapy, which is often used to treat brain tumors like gliomas or metastases. While radiation targets cancer cells, it can also harm healthy brain tissue over time. This injury can lead to problems like memory loss, confusion, or even more severe issues like brain necrosis, where tissue dies off. It’s a delayed complication, meaning symptoms might not show up right away, sometimes taking months or even years to appear, and it can really affect a patient’s quality of life.
Why do you think RIBI is becoming more common despite advancements in radiotherapy techniques?
That’s a great question. Modern radiotherapy has indeed become more precise with techniques like stereotactic radiosurgery, which focus radiation more tightly on tumors and spare healthy tissue. Plus, survival rates for brain cancer patients have improved, so more people are living longer after treatment. But here’s the catch: with longer survival, there’s more time for delayed side effects like RIBI to develop. Also, even with better targeting, some radiation still reaches surrounding brain tissue, and over time, that cumulative exposure can cause damage, especially in sensitive areas.
How does RIBI typically affect a patient’s everyday life, particularly in terms of brain function and well-being?
RIBI can have a profound impact. In the early stages, patients might feel fatigued, have headaches, or struggle with mild confusion. As it progresses, especially in the later phases, they could face serious cognitive challenges—trouble with memory, difficulty concentrating, or even problems with decision-making. This can make simple tasks like managing finances or holding a conversation really hard. Emotionally, it’s tough too; patients often deal with frustration or depression because they can’t function like they used to. Physically, symptoms like seizures can further disrupt their daily routine, affecting their independence and overall happiness.
What happens to the blood-brain barrier during radiation exposure, and why is that such a big issue?
The blood-brain barrier, or BBB, is like a protective shield that controls what enters the brain from the bloodstream. When radiation hits the brain, it damages the tiny blood vessels and the cells lining them, making the BBB more permeable—or leaky. This allows inflammatory substances and immune cells to slip into the brain tissue, which normally wouldn’t happen. That leakage triggers swelling and inflammation, which can harm neurons and other brain cells, contributing to symptoms like cognitive decline. It’s a big issue because once the BBB is compromised, it’s harder for the brain to maintain its delicate balance and recover from injury.
How does inflammation in the brain play a role in the damage caused by radiation?
Inflammation is a key player in RIBI. When radiation damages brain tissue, it activates cells called microglia and astrocytes, which are part of the brain’s immune system. These cells release pro-inflammatory chemicals, known as cytokines, like IL-6 and IL-1β. While this response is meant to protect and repair, in RIBI, it often goes overboard, causing a chronic inflammatory state. This ongoing inflammation can lead to the death of neurons and disrupt normal brain signaling, which is why patients experience issues like memory loss or trouble thinking clearly. It’s a vicious cycle that amplifies the initial radiation damage.
Can you shed light on how oxidative stress contributes to RIBI and its effects on brain cells?
Sure. Oxidative stress happens when radiation generates reactive oxygen species, or ROS, which are highly unstable molecules. These ROS can damage pretty much every part of a cell—its DNA, proteins, and membranes. In the brain, this is especially harmful because neurons don’t regenerate easily. The damage can cause DNA breaks, mess up protein functions, and impair the cell’s ability to repair itself. Over time, this leads to cell death and contributes to the broader tissue damage we see in RIBI, manifesting as cognitive and neurological problems for the patient.
What kind of damage does radiation cause to white matter, and how does that impact thinking and memory?
White matter is the part of the brain made up of nerve fibers that connect different regions, kind of like the brain’s wiring. Radiation can cause demyelination, which is the loss of the protective coating around these fibers, and even axonal loss, where the fibers themselves break down. When this happens, the signals between brain areas slow down or get disrupted. Since white matter is crucial for processes like memory, learning, and executive functions, this damage often results in difficulties with recalling information, solving problems, or multitasking. It’s one of the reasons RIBI can be so debilitating over time.
Are there genetic factors that make some individuals more prone to developing RIBI?
Yes, there’s growing evidence that genetics play a role. Certain variations, or polymorphisms, in specific genes can influence how someone’s brain responds to radiation. For instance, differences in genes related to DNA repair or inflammation pathways can make some people more vulnerable to damage from radiation exposure. While research is still ongoing, identifying these genetic markers could help us predict who’s at higher risk for RIBI before starting treatment, allowing for more tailored approaches to therapy or closer monitoring afterward.
How has advanced imaging changed the way we detect and diagnose RIBI compared to traditional methods?
Advanced imaging has been a game-changer. Traditional MRI is great for spotting obvious changes like swelling or necrosis, but it often can’t catch RIBI early or distinguish it from tumor recurrence. Now, with multimodal imaging techniques like diffusion imaging, perfusion imaging, and metabolic scans such as MRS or PET/CT, we can look at the brain’s microstructure, blood flow, and even chemical composition. These tools give us a much clearer picture of whether a lesion is due to radiation damage or cancer coming back, and they help us detect subtle changes long before symptoms become severe, which is critical for early intervention.
What are some of the most promising therapeutic strategies for managing RIBI right now?
We’re moving beyond just managing symptoms with steroids, which can have nasty side effects over time, to more targeted treatments. One standout is bevacizumab, a drug that blocks a protein involved in blood vessel growth. It’s been shown in trials to help with radiation necrosis by reducing swelling and tissue damage. Other approaches, like hyperbaric oxygen therapy, aim to boost tissue repair by increasing oxygen levels in the brain. There’s also exciting research into stem cell therapy and even neuromodulation techniques like transcranial magnetic stimulation to aid cognitive recovery. While some of these are still experimental, they’re paving the way for more effective, personalized care.
What do you foresee for the future of RIBI treatment and diagnosis over the next decade?
I’m optimistic about where we’re headed. I think we’ll see a big push toward precision medicine for RIBI—using genetic and imaging data to predict who’s at risk and customize treatments before damage even starts. Biomarker discovery will likely play a huge role, giving us early warning signs we can act on. I also expect artificial intelligence to become more integrated into imaging analysis, making diagnoses faster and more accurate. On the treatment side, therapies targeting specific mechanisms like inflammation or oxidative stress could become standard, and I hope to see more clinical trials validating innovative approaches like stem cell therapy. Ultimately, the goal is to prevent RIBI or minimize its impact, and I believe the next decade will bring us much closer to that.