The pharmaceutical industry confronts an enduring challenge where the path to a single approved therapy is fraught with immense financial risk, extended timelines, and a staggeringly high rate of failure in late-stage clinical trials. This high-attrition model is becoming increasingly unsustainable, creating immense pressure to innovate the fundamental processes of drug discovery and development. In response, a strategic pivot toward a more precise, data-centric paradigm is gaining momentum, driven by the transformative power of biomarkers. These biological indicators, particularly protein biomarkers, have evolved far beyond their traditional role as simple research tools to become indispensable strategic assets. By offering profound biological insights at every critical decision point, biomarker-driven strategies provide a direct and powerful solution to de-risk the entire development lifecycle, enabling a “fail-fast” philosophy for non-viable candidates while maximizing the potential for success and conserving vast resources.
Strengthening the Foundation in Early-Stage Discovery
Pinpointing the Right Targets with Deeper Biology
A principal cause of costly late-stage failures originates at the very beginning of the development pipeline: poor target selection due to an incomplete understanding of a target’s biological relevance. Protein biomarkers offer a direct and functional window into the complex mechanisms of disease, empowering research and development teams to select targets with a more robust scientific foundation and a significantly higher probability of translating into clinical success. This is achieved through a multiomics approach, which integrates dynamic proteomics data with the more static information from genomics and transcriptomics. While genomics can identify genetic predispositions, proteomics captures the real-time protein activity that drives the disease process. This comprehensive, multi-layered view of disease biology provides a much richer context for target identification and validation, moving beyond simple correlation to a deeper understanding of causation and ensuring that development programs are built on the most promising and biologically sound foundations.
Creating a Data-Driven Feedback Loop
Modern drug development is increasingly leveraging a powerful strategy known as reverse translation, which establishes a direct feedback loop from human clinical data back to early-stage research. By analyzing proteomic data gathered from patients participating in clinical trials, scientists can observe precisely how a drug candidate modulates biological pathways within the human body. This invaluable feedback is then used to inform and refine upstream discovery decisions, enabling better prioritization of future targets and supporting the swift discontinuation of candidates that fail to effectively engage their intended molecular pathways. This iterative process fundamentally reduces downstream risk by ensuring that only the most biologically active and mechanistically sound candidates are advanced through the development pipeline. It transforms drug development from a linear, high-risk cascade into a dynamic, learning system where each clinical study provides actionable intelligence to de-risk subsequent programs and improve the overall efficiency of the R&D engine.
Optimizing the Path to Approval in Clinical Trials
Enabling Smarter and Faster Decisions
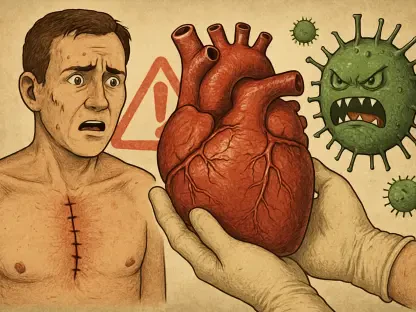
Beyond the initial discovery phase, biomarkers are fundamentally transforming the design, execution, and interpretation of clinical trials by delivering objective, real-time data on a drug’s performance and its effects on patients. Proteomic biomarkers, in particular, can serve as direct and early indicators of a drug’s biological activity. They provide clear evidence of target engagement, confirming that the drug is interacting with its intended molecular target, and measure pathway modulation, revealing the downstream biological consequences of that engagement. Access to this critical information early in clinical development, such as in Phase I trials, empowers teams to make rapid and well-informed go/no-go decisions. This capacity embodies a “fail-fast” strategy that prevents organizations from committing hundreds of millions of dollars and several years to a therapeutic candidate that is ultimately ineffective, thereby optimizing resource allocation and focusing efforts on the most promising assets.
From Fail-Fast Strategies to Precision Medicine
Many diseases that present with similar clinical symptoms are, in fact, highly heterogeneous at the molecular level, a complexity that has historically contributed to trial failures when a “one-size-fits-all” approach is used. Proteomics provides the high-resolution tools needed to uncover these underlying biological differences within a patient population, enabling the precise stratification of individuals into distinct subgroups. By identifying the patients who are most likely to respond to a particular therapy based on their unique molecular profile, trial sponsors can design more targeted, efficient studies with a significantly improved probability of a successful outcome. This approach is a cornerstone of precision medicine, ensuring that therapies are matched to the specific biological drivers of a patient’s disease. It not only increases the likelihood of regulatory approval but also leads to more meaningful clinical benefits and better outcomes for patients by delivering the right treatment to the right person.
Improving the Trial Experience and Outcome
Historically, clinical trials for many diseases, especially those affecting internal organs, have relied on invasive biopsies to measure treatment efficacy, a process that is often burdensome for patients and can deter trial participation. Blood-based protein biomarkers are emerging as powerful and non-invasive alternatives that can revolutionize the patient experience. These biomarkers can be measured frequently and easily from a simple blood draw, drastically reducing the physical and logistical burden on participants, which in turn can help accelerate trial recruitment and improve retention rates. Moreover, modern high-throughput proteomic platforms can quantify thousands of proteins from very small sample volumes, maximizing the data generated from each precious biological sample. This capability ensures that researchers can gain deeper biological insights and make more robust, evidence-based decisions without depleting irreplaceable patient material, ultimately leading to faster and more comprehensive readouts of a drug’s effect.
A New Era of Evidence-Based Development
The strategic integration of biomarkers, particularly those derived from advanced proteomics, has shifted from an optional enhancement to an essential component of modern and successful drug development. These biological indicators provided a cohesive, evidence-based framework that connected the dots between fundamental disease biology, a drug’s mechanism of action, and the ultimate clinical outcomes observed in patients. By delivering actionable insights at every critical stage, this biomarker-driven approach directly confronted the industry’s most significant challenges, offering a clear path toward reducing development risk and improving the objectivity of decision-making. This strategic shift fundamentally elevated the role of biomarkers from merely supportive tools to core drivers of innovation, efficiency, and success.