The 2022 mpox outbreak served as a stark reminder of our vulnerability to emerging infectious diseases. While existing smallpox vaccines offered a line of defense, they were a cumbersome tool against a rapidly spreading threat. Now, a stunning breakthrough powered by artificial intelligence has identified a new target on the monkeypox virus, paving the way for simpler, more effective vaccines and treatments. We sat down with biopharma expert Ivan Kairatov to discuss how researchers are using AI to reverse-engineer nature’s defenses, the practical advantages of this new single-protein approach over traditional vaccines, and what this discovery means for our future preparedness against both mpox and the lingering threat of smallpox.
You mentioned it would have taken years to find the OPG153 target protein without AI. Could you describe the traditional methods you would have used and then walk us through, step-by-step, how the AlphaFold model accelerated this specific discovery process for the monkeypox virus?
Absolutely. Traditionally, this would have been a monumental task of brute-force biology. Imagine you have 12 highly effective antibodies, but you don’t know what they’re attacking on the virus. The monkeypox virus has dozens of proteins on its surface, maybe 35 or so. The old method would have required us to individually produce and purify every single one of those proteins in the lab. Then, we would have had to run complex and sensitive binding experiments for each of the 12 antibodies against each of the 35 proteins. It’s a massive, resource-intensive matrix of experiments that is not only expensive but, as the researchers said, could easily take years of meticulous, often frustrating, lab work.
With AI, the process was completely transformed. The AlphaFold model acted as a brilliant computational shortcut. Instead of physically making and testing everything, the Texas team could digitally model the 3D structures of all the viral proteins and the patient-derived antibodies. The AI then predicted, with a very high degree of confidence, which protein the antibodies were most likely to bind to. It essentially sifted through all the possibilities in silico and pointed a giant arrow directly at OPG153. This turned a years-long discovery mission into a focused, rapid verification process. The lab work wasn’t eliminated, but it became about confirming a single, high-probability target rather than searching blindly for a needle in a haystack.
The article describes your method as “reverse vaccinology,” starting with 12 antibodies from recovered patients. Can you elaborate on the key milestones in that process, from isolating those antibodies to the moment you experimentally confirmed OPG153 as the correct antigen target?
This “reverse vaccinology” approach is incredibly elegant because it starts with a successful outcome and works backward. The first milestone is really about trusting the human immune system. Instead of guessing which part of the virus might make a good vaccine, the researchers went to people who had already recovered from mpox or been vaccinated. Their bodies had already solved the puzzle and produced antibodies capable of neutralizing the virus. The second key milestone was the painstaking work done in Italy to isolate these “champion” antibodies from patient blood samples and identify the 12 most potent ones.
This created the central mystery: what were these powerful antibodies actually targeting? That’s where the AI-driven step became the third, and arguably most pivotal, milestone. The prediction that OPG153 was the target was a watershed moment. But the final, most satisfying milestone was the experimental confirmation. There’s always a palpable sense of excitement in the lab when you move from a computer model to a real-world result. When the follow-up experiments showed that the antibodies did, in fact, bind strongly to OPG153, it validated the entire chain of logic, from the patient’s immune response all the way to the AI’s prediction. It’s the moment the digital hypothesis becomes a biological fact.
The innovation is described as a “single protein that’s easy to make” versus a complex whole-virus vaccine. What are the practical differences in manufacturing, and can you provide any potential metrics on the cost, scalability, or speed advantages this new approach might offer global health initiatives?
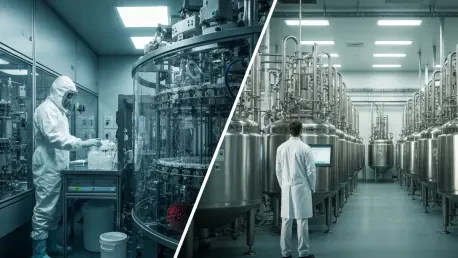
The difference in manufacturing is like night and day. A whole-virus vaccine, like the one repurposed for mpox, involves growing a live, albeit weakened, virus. This requires specialized, high-containment biosafety facilities. It’s a slow, biologically complex process that is difficult to scale up quickly and carries inherent risks that must be carefully managed. Think of it as cultivating a delicate, dangerous orchid. It’s complicated and costly.
A single-protein vaccine, on the other hand, is far more straightforward. You just need the genetic code for that one protein, OPG153 in this case. You can then insert that code into robust, well-established manufacturing platforms, like yeast or bacteria, and have them produce vast quantities of the protein in large bioreactors. This is standard, safe, and highly scalable biotechnology. This approach dramatically lowers production costs and, most importantly, accelerates the timeline. In a public health crisis, the ability to rapidly produce millions of doses in facilities around the world, rather than in a few specialized labs, is a game-changer for ensuring equitable access and containing an outbreak.
Beyond monkeypox, the research points to a potential new defense against smallpox. What are the immediate next steps in developing the OPG153 protein as a viable vaccine candidate, and what specific challenges must be overcome to translate these promising results in mice to human clinical trials?
The immediate next steps are focused on refinement and rigorous testing. The team is likely engineering optimized versions of the OPG153 protein to make it even better at stimulating a protective immune response. Simultaneously, they’ll be developing the therapeutic antibodies to be more effective and have a longer shelf life. This is all crucial preclinical work that lays the foundation for human trials.
The greatest challenge is always translating success in animal models to humans. The phrase we often use is crossing the “valley of death” in drug development. While the results in mice are incredibly promising, the human immune system is far more complex. The path forward involves a very methodical and heavily regulated process: Phase 1 trials to establish safety, followed by larger Phase 2 and 3 trials to prove efficacy. This requires significant funding, navigating complex regulatory approvals from agencies like the FDA, and manufacturing the vaccine candidate under strict quality-controlled conditions. Given that smallpox is considered a high-risk bioterrorism threat, there will be immense interest and support, but the scientific and regulatory bar for a new vaccine is, and should be, exceptionally high.
What is your forecast for the role of AI in vaccine development over the next decade?
I believe we are at the very beginning of a revolution. What we’ve seen here with mpox will transition from being a novel breakthrough to the standard operating procedure for vaccine development. In the next decade, AI will not only be used to identify existing targets on pathogens but will be used for de novo design—creating entirely new vaccine antigens from scratch that are more potent, stable, and safer than anything nature has produced. AI will also become indispensable in predicting clinical trial outcomes, helping researchers prioritize the most promising candidates and avoid costly late-stage failures. This will radically shorten development timelines, from years to potentially months. My forecast is a future where our response to a new pandemic threat is not a frantic, multi-year race, but a rapid, precise, and AI-guided design process.