I’m thrilled to sit down with Ivan Kairatov, a renowned biopharma expert whose extensive experience in research and development, paired with a passion for technology and innovation, has positioned him at the forefront of transformative advancements in the industry. Today, we’ll dive into the groundbreaking work happening at Cellarity, a clinical-stage biotech company focused on Cell State-Correcting therapies. Our conversation will explore the critical challenge of drug-induced liver injury (DILI), the role of AI in predictive toxicology, and how cutting-edge tools like ToxPredictor are reshaping drug safety evaluations. We’ll also touch on the power of toxicogenomics and the impact of open-source data in driving collaboration and innovation in drug development.
Can you start by telling us about Cellarity and its mission to pioneer Cell State-Correcting therapies?
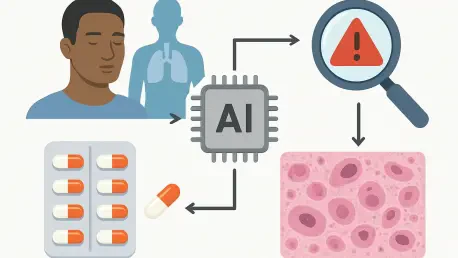
Absolutely, Julia. Cellarity is a clinical-stage biotech company dedicated to transforming how we approach disease by focusing on cell behavior rather than single molecular targets. Our mission is to develop Cell State-Correcting therapies, which means we aim to correct dysfunctional cellular states that underlie many complex diseases. By integrating multi-omics data and AI modeling, we’re able to map and manipulate cell behavior in ways that open up new therapeutic possibilities, especially in areas with significant unmet needs like drug safety challenges.
What led Cellarity to zero in on drug-induced liver injury, or DILI, as a key focus area in drug development?
DILI is one of the biggest hurdles in drug development today. It’s a leading cause of clinical trial failures and even market withdrawals when liver safety issues emerge late in the process or post-approval. The liver is such a critical organ, metabolizing drugs and often bearing the brunt of toxic effects. We saw an opportunity to address this gap in preclinical testing, where current methods often miss these risks, and use our expertise in AI and multi-omics to create a solution that could save time, costs, and most importantly, protect patient safety.
Why is DILI such a persistent challenge for the pharmaceutical industry, and how often do traditional models fall short?
The challenge with DILI lies in its complexity. It can manifest in various ways—acute injury, chronic damage, or even subtle metabolic disruptions—and often isn’t detected until human trials or beyond. Traditional animal models, while useful, fail to identify up to half of the drugs linked to DILI in humans because of species-specific differences in liver metabolism and response. This gap creates a huge risk for developers and patients alike, driving the need for more predictive, human-relevant approaches like the ones we’re pioneering.
Can you walk us through ToxPredictor and how it leverages AI to assess DILI risks?
ToxPredictor is an integrated AI model we’ve developed to predict dose-related DILI risks with high accuracy. It uses a combination of machine learning and toxicogenomics—essentially analyzing gene expression changes in response to drug exposure—to evaluate potential liver toxicity. By training on vast datasets of transcriptional signatures from human liver cells, ToxPredictor can identify patterns linked to DILI long before traditional signs of damage appear. It’s like having a high-resolution early warning system for liver safety.
What sets the DILImap dataset apart, and why is it considered a breakthrough in toxicogenomics research?
DILImap is the backbone of ToxPredictor and represents the largest known toxicogenomics dataset for DILI modeling. It captures the transcriptional signatures of 300 compounds associated with liver injury, tested at multiple concentrations in primary human hepatocytes. This breadth and depth allow us to map a wide range of toxicity profiles and mechanisms, making it a unique resource. It’s a game-changer because it shifts us away from animal-based predictions toward human-relevant data, aligning with regulatory pushes to reduce animal testing.
How was the DILImap library created, and what kind of scope does it cover?
Building DILImap was a massive undertaking. We exposed primary human liver cells to 300 compounds known to be linked with DILI, testing each at various concentrations to capture dose-dependent effects. We then used advanced sequencing to analyze the transcriptional changes—basically, how the cells’ gene expression shifted in response to each compound. This library covers a spectrum of chemical structures and toxicity mechanisms, providing a comprehensive dataset that reflects real-world drug exposure scenarios.
ToxPredictor achieved an 88% sensitivity at 100% specificity in blind testing. Can you break down what these figures mean for a general audience and why they’re significant?
Sure, Julia. Sensitivity measures how well the model detects true DILI risks—in this case, it correctly identified 88% of compounds that cause liver injury. Specificity, at 100%, means it didn’t falsely flag any safe compounds as toxic. These numbers are significant because they show ToxPredictor is both highly accurate in catching real dangers and extremely reliable in avoiding false alarms, which is critical for drug developers who need trustworthy tools to make go/no-go decisions early on.
How does ToxPredictor stack up against traditional preclinical safety models, especially given its superior performance over many industry standards?
ToxPredictor has outperformed over 20 industry-standard preclinical safety models in head-to-head comparisons. Traditional models often rely on animal testing or simpler in vitro assays that focus on narrow endpoints like cell death. In contrast, ToxPredictor uses the full transcriptomic landscape—thousands of gene expression data points—to predict a broader range of DILI risks. This allows it to catch issues that slip through the cracks in conventional testing, including late-stage clinical failures that animal studies missed.
Can you share an insight into the liver toxicity mechanisms that ToxPredictor helps uncover, such as mitochondrial dysfunction or oxidative stress?
Absolutely. One of the strengths of ToxPredictor is its ability to pinpoint specific mechanisms driving liver toxicity. For instance, it can detect mitochondrial dysfunction, where a drug disrupts the energy-producing parts of liver cells, leading to cellular stress and damage. It also identifies oxidative stress, which happens when harmful reactive molecules build up and overwhelm the cell’s defenses. Understanding these pathways helps developers tweak compounds or adjust dosing to minimize risks before they become clinical problems.
Why did Cellarity choose to make ToxPredictor and its validation data open-source, and how do you think this will influence the drug development field?
We decided to make ToxPredictor and its validation data publicly available because we believe collaboration is key to accelerating progress in drug safety. By sharing these resources, we’re enabling other researchers, developers, and even regulators to use and build upon our work. This open-source approach can de-risk drug candidates across the industry, reduce redundant efforts, and ultimately foster a shift toward more predictive, human-focused safety evaluations. It’s about creating a rising tide that lifts all boats.
How do you envision ToxPredictor shaping the future of drug safety evaluations, especially with growing regulatory emphasis on reducing animal testing?
I see ToxPredictor as a catalyst for a paradigm shift in drug safety. With regulators worldwide pushing to minimize animal testing, tools like ours—grounded in human-relevant data and AI—offer a viable alternative that’s not only more ethical but also more accurate. Over time, I believe models like ToxPredictor will become integral to preclinical workflows, helping developers screen compounds earlier, refine candidates with precision, and bring safer drugs to market faster. It’s a future where technology and patient safety go hand in hand.
What is your forecast for the role of AI and toxicogenomics in the broader landscape of drug development over the next decade?
I’m incredibly optimistic about the trajectory of AI and toxicogenomics in drug development. Over the next decade, I predict these technologies will become foundational, not just for safety assessments like DILI but across the entire drug discovery pipeline—from target identification to personalized medicine. AI will enable us to integrate and interpret complex biological data at an unprecedented scale, while toxicogenomics will provide the molecular insights needed to predict and prevent adverse effects. Together, they’ll drive a more efficient, cost-effective, and patient-centric approach, fundamentally transforming how we create new therapies.