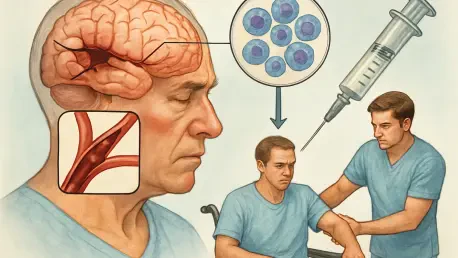
Imagine a world where millions of stroke survivors, left with debilitating long-term disabilities, find renewed hope through a groundbreaking treatment that repairs brain damage long after the critical hours have passed, offering a chance at recovery previously thought impossible. Stroke, a leading cause of death and disability globally, affects countless lives each year, with ischemic strokes—caused by blocked blood flow to the brain—making up nearly 90% of cases. Current treatments are often limited by a narrow four-and-a-half-hour window, leaving many without options. This roundup dives into the emerging field of stem cell therapy, gathering insights, opinions, and research perspectives from various experts and studies to explore whether this innovative approach could revolutionize stroke recovery. By compiling diverse viewpoints, the aim is to shed light on the potential, challenges, and future directions of this promising medical frontier.
Uncovering the Promise of Stem Cell Therapy in Stroke Treatment
Stem cell therapy has emerged as a beacon of hope for addressing the unmet needs in stroke care, particularly for patients who miss the acute intervention window. Many researchers highlight the therapy’s potential to regenerate damaged brain tissue, a feat unattainable by conventional treatments like clot removal. Reports from multiple scientific discussions suggest that stem cells could offer a paradigm shift by focusing on long-term recovery rather than just immediate damage control, sparking optimism across the medical community.
Differing opinions exist on the readiness of this approach for widespread use. Some experts argue that preclinical studies show remarkable promise, with animal models demonstrating both structural brain repair and functional improvements. Others caution that human application remains a distant goal due to complexities in brain function and the need for extensive safety validations. This diversity in thought underscores the importance of continued exploration and dialogue in the field.
A common thread among various analyses is the emphasis on bridging the gap between theory and practice. Commentators from neuroscience forums note that while the concept of using stem cells to rebuild neural networks is exciting, the practical challenges of scalability and patient-specific responses cannot be overlooked. These insights set the stage for a deeper examination of specific research findings and expert perspectives on how stem cell therapy might evolve.
Deep Dive into Research and Opinions on Stem Cell Therapy
Insights on Neural Stem Cell Transplants from Preclinical Studies
Recent studies involving neural stem cell transplants in animal models have garnered significant attention for their encouraging results. Findings from multiple research groups indicate that transplanting stem cells derived from reprogrammed human cells into stroke-damaged brains of mice can lead to notable recovery. Observations include reduced inflammation and enhanced growth of neurons, suggesting a reparative effect on brain tissue even weeks after a stroke event.
Skepticism persists among some scientists regarding the translation of these results to human patients. Commentators in academic reviews point out that the human brain’s complexity and variability pose unique challenges not fully replicated in animal models. Concerns about immune responses and the long-term integration of transplanted cells are frequently raised, highlighting a cautious stance on immediate clinical expectations.
A balanced perspective shared by several research summaries is the need for rigorous testing over extended periods. Experts advocate for studies spanning from the current year to at least 2027 to assess the durability of these transplanted cells. Such long-term data is deemed essential to determine whether initial successes in preclinical settings can withstand the test of time and real-world variables.
Functional Outcomes and Real-World Implications
Beyond structural repair, the functional recovery observed in treated animal models has fueled discussions on stem cell therapy’s practical impact. Multiple reports detail how treated subjects regained motor skills, with some demonstrating restored coordination in complex tasks within weeks. These outcomes, often measured using advanced analytical tools, point to tangible benefits that could enhance quality of life for stroke survivors.
Divergent views emerge on interpreting these functional gains for human application. Some medical professionals express optimism, suggesting that even partial restoration of movement or cognition could be life-changing for patients with chronic disabilities. Others warn against over-enthusiasm, noting that animal behavior may not fully mirror human recovery needs, particularly in areas like speech or emotional regulation affected by stroke.
An often-cited concern in expert roundtables is the balance between hope and realism. While the potential to address long-term stroke damage is undeniable, many stress the importance of managing patient expectations. The consensus leans toward viewing these early functional improvements as a stepping stone, prompting calls for more comprehensive studies to validate real-world effectiveness across diverse patient groups.
Cellular Mechanisms and Therapeutic Pathways
Understanding how stem cells interact with the brain post-stroke is a focal point of current research discussions. Insights from various scientific analyses reveal that transplanted cells often adapt to the brain’s environment, with many differentiating into specific neuron types crucial for regulating brain activity. This adaptability is seen as a key driver of neural regeneration and connectivity restoration.
Opinions differ on how these cellular mechanisms can be harnessed for broader therapeutic strategies. Some researchers propose targeting specific signaling pathways activated by stem cells to develop complementary drug treatments, enhancing recovery outcomes. Others argue that such an approach might oversimplify the intricate dynamics of brain repair, advocating for personalized therapies tailored to individual stroke profiles and severities.
A recurring theme in expert commentary is the challenge of standardizing these mechanisms for clinical use. Discussions in medical journals emphasize that variability in patient responses and stroke types necessitates a nuanced understanding of cellular interactions. This complexity fuels ongoing debates on whether stem cell therapy can truly become a universal solution or if it must remain a highly customized intervention.
Challenges in Translating Lab Success to Clinical Reality
The journey from lab results to bedside application is fraught with hurdles, as noted by numerous stakeholders in regenerative medicine. Many highlight that while animal studies show promise, human trials must address critical issues like cell viability over a lifetime and potential adverse effects. This perspective calls for a cautious yet proactive approach to clinical translation.
Ethical and regulatory barriers also feature prominently in expert analyses. Some voices in the field stress that the use of stem cells raises significant ethical questions, particularly around sourcing and consent, which could delay progress. Others counter that streamlined regulatory frameworks, informed by global collaboration, could accelerate safe adoption without compromising patient welfare.
A shared viewpoint among various research summaries is the need for interdisciplinary efforts to overcome these obstacles. Combining expertise from neuroscience, bioethics, and policy-making is often recommended to ensure that stem cell therapy advances responsibly. This collaborative mindset is seen as vital to navigating the intricate path from experimental success to tangible patient benefits.
Key Takeaways from Diverse Perspectives
Synthesizing the range of opinions, it’s clear that stem cell therapy holds transformative potential for stroke recovery, especially for those beyond the acute treatment window. Studies consistently point to structural and functional improvements in preclinical models as a foundation for hope. However, the spectrum of views—from enthusiastic support to measured caution—reflects the complexity of moving this therapy into human application.
A notable divergence lies in the timeline and scope of clinical readiness. While some experts push for accelerated trials to meet urgent patient needs, others advocate for prolonged preclinical research to iron out uncertainties. This tension underscores a broader agreement on the necessity of robust funding and international cooperation to refine methodologies and ensure safety.
Practical guidance from these discussions often centers on fostering public and professional awareness. Many suggest that stakeholders, including healthcare providers and policymakers, should prioritize education on stem cell therapy’s current state. Staying updated on trial progress and supporting advocacy for innovative treatments are frequently cited as actionable steps to drive this field forward.
Reflecting on the Path Ahead
Looking back on the insights gathered, the exploration of stem cell therapy for stroke recovery revealed a landscape of immense potential tempered by significant challenges. The collective wisdom from various research efforts and expert opinions painted a picture of cautious optimism, where early successes in animal models laid a promising groundwork. Diverse perspectives highlighted both the excitement of brain repair possibilities and the sobering realities of clinical translation.
Moving forward, a critical next step involves amplifying investment in long-term studies to validate the durability and safety of stem cell interventions. Encouraging global partnerships among scientists, ethicists, and regulators emerged as a pivotal strategy to address barriers and standardize practices. Additionally, fostering dialogue between medical communities and the public could help align expectations with realistic outcomes, paving the way for informed support of this evolving field.