Every day, millions of families worldwide grapple with the devastating effects of Alzheimer’s disease, a condition that robs individuals of their memories and independence, leaving loved ones searching for answers and desperate for solutions. With over 50 million people affected globally and numbers projected to rise, the urgency for innovative treatments has never been greater. This roundup dives into a groundbreaking discovery about a specific subtype of microglia—the brain’s immune cells—that could potentially shield against Alzheimer’s progression. By gathering insights, opinions, and perspectives from various scientific communities and research efforts, this discussion aims to illuminate the promise and challenges of this finding, offering a comprehensive look at what it might mean for future therapies.
Uncovering Microglia’s Dual Nature: A Shift in Perspective
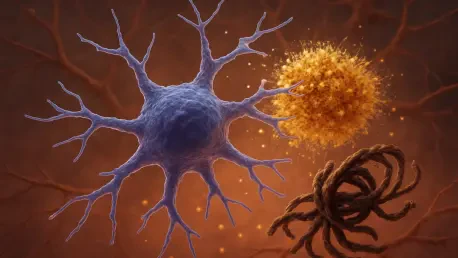
The scientific community has long debated the role of microglia in Alzheimer’s, often viewing these cells as contributors to inflammation and neurodegeneration. However, recent research has sparked a shift, highlighting a subset of microglia that may act as protectors rather than aggressors. Reports from multiple neuroscience forums suggest that this subtype, characterized by unique molecular markers, could reduce the buildup of harmful amyloid plaques and tau protein tangles—hallmarks of Alzheimer’s pathology. This emerging consensus challenges traditional views and has ignited excitement among researchers eager to explore new therapeutic avenues.
A variety of opinions exist on how this discovery alters the landscape of Alzheimer’s research. Some experts in neuroimmunology argue that understanding microglial diversity is key to unlocking treatments that modulate brain inflammation without causing collateral damage. Others caution that while the protective potential is promising, the complexity of microglial behavior across different stages of the disease remains a significant hurdle. These differing stances underscore the need for broader studies to validate early findings and ensure practical applications.
Molecular Mechanisms: Insights into Protective Pathways
The PU.1-CD28 Axis: A Game-Changer?
Delving into the specifics, a recurring theme across research discussions is the identification of a molecular framework involving reduced PU.1 expression and active CD28 receptors in this microglia subtype. Scientific analyses from various institutions highlight how lowering PU.1—a transcription factor—seems to enhance immunoregulatory functions, enabling microglia to curb neuroinflammation. Meanwhile, CD28, a receptor typically associated with immune responses in other cell types, appears to play a pivotal role in maintaining this protective state, based on experimental outcomes shared in academic circles.
Contrasting perspectives emerge when evaluating the feasibility of targeting this PU.1-CD28 axis. Some researchers express optimism, pointing to animal model studies that demonstrate slowed disease progression and improved cognitive outcomes when this pathway is activated. However, others raise concerns about the risks of manipulating such intricate molecular interactions, warning of potential unintended immune responses that could exacerbate conditions if not carefully controlled. This debate reflects a cautious yet hopeful outlook on translating these mechanisms into human therapies.
A third angle focuses on the scalability of these findings. Discussions in scientific panels suggest that while the molecular insights are compelling, the small population of these protective microglia in the brain poses a challenge for therapeutic design. Strategies to amplify their effects or mimic their behavior through drugs are under exploration, but consensus on the best approach remains elusive, fueling ongoing investigations.
Bridging Disciplines: Immunology Meets Neuroscience
Another fascinating dimension is the intersection of immunology and neuroscience in understanding this microglia subtype. Insights gathered from interdisciplinary conferences reveal a growing appreciation for how principles from immune cell regulation can inform brain health strategies. The involvement of CD28, a receptor borrowed from T-cell biology, has intrigued many in the field, with some suggesting that shared regulatory mechanisms across immune cells could inspire novel immunotherapies for Alzheimer’s.
Differing opinions surface on the pace of integrating these cross-disciplinary approaches. Certain factions within the research community advocate for rapid clinical trials to test therapies inspired by these findings, emphasizing the urgency of addressing Alzheimer’s burden. Conversely, a more conservative view stresses the importance of extensive preclinical research to fully grasp the long-term implications of altering microglial states, highlighting potential risks of immune system dysregulation.
Additionally, global research networks have noted the value of collaborative efforts in advancing this field. Perspectives from various regional hubs indicate that pooling resources and expertise across borders has accelerated the understanding of microglia’s role, with funding bodies like national health institutes playing a critical part. This collective push underscores a shared commitment to turning theoretical insights into tangible solutions for patients.
Therapeutic Horizons: What Experts Envision
Microglia as Targets: Opportunities and Obstacles
Looking toward therapeutic possibilities, a spectrum of ideas emerges from research symposiums about harnessing microglia for Alzheimer’s treatment. Many in the scientific community see the plasticity of microglial states as fertile ground for innovation, proposing that drugs or biologics could nudge these cells into a protective mode. This optimism is tempered by logistical challenges, such as delivering interventions to specific brain regions without triggering adverse effects.
Alternative viewpoints focus on combining microglia-targeting strategies with existing Alzheimer’s therapies. Some experts suggest that integrating these approaches with anti-amyloid drugs could yield synergistic benefits, enhancing overall efficacy. Others argue that standalone microglia-based treatments might face fewer compatibility issues, advocating for a focused development pipeline. These contrasting strategies highlight the diversity of thought in crafting the next generation of Alzheimer’s interventions.
A broader concern raised in research circles is the accessibility of such therapies once developed. Discussions point to the need for cost-effective solutions that can reach diverse populations, especially in under-resourced areas. This priority reflects a growing awareness that scientific breakthroughs must be paired with practical implementation plans to truly impact global health outcomes.
Global Efforts and Future Directions
The international scope of this research has garnered attention across multiple platforms, with regional efforts showcasing varied approaches to studying microglia. Updates from collaborative projects reveal that funding and policy support from governmental and academic bodies are driving progress, with initiatives spanning from 2025 to 2027 aimed at mapping microglial diversity in human brains. These efforts are seen as crucial for validating findings across different demographics and disease contexts.
Opinions on the timeline for clinical impact differ significantly. While some research groups anticipate breakthroughs in therapeutic applications within the next decade, others adopt a more measured stance, emphasizing that foundational questions about microglial behavior must be resolved first. This variance in expectations illustrates the complexity of moving from lab discoveries to bedside solutions, a process that requires patience and persistence.
A unifying theme across these discussions is the call for public engagement and education. Many in the field stress that informing communities about emerging Alzheimer’s research can foster support for funding and participation in clinical trials. This push for awareness aims to bridge the gap between scientific advancements and societal benefit, ensuring that progress reaches those who need it most.
Reflecting on the Journey: Next Steps for Alzheimer’s Research
Looking back, the exploration of a protective microglia subtype marked a pivotal moment in Alzheimer’s research, as it reshaped perceptions of the brain’s immune cells from foes to potential allies. The diverse insights gathered from scientific communities worldwide painted a picture of cautious856 optimism, balancing the excitement of molecular discoveries with the realities of therapeutic challenges. This collective dialogue underscored the importance of interdisciplinary collaboration in tackling a disease that affects millions.
Moving forward, the focus shifts to actionable strategies, such as prioritizing the development of microglia-targeting immunotherapies and fostering global partnerships to pool expertise. A critical next step involves investing in longitudinal studies to track how these protective cells behave over time in human patients, providing data to refine treatment approaches. Additionally, advocating for increased funding and policy support emerges as a vital consideration to sustain momentum in this promising field, ensuring that hope translates into help for those battling Alzheimer’s.