What if a simple eye scan could forecast a patient’s risk of losing vision to a stealthy, progressive condition long before irreversible damage sets in, offering a lifeline to preserve sight? This question is no longer a distant dream but a tangible reality emerging in the field of ophthalmology. At a recent gathering of global eye care experts, a groundbreaking study unveiled artificial intelligence (AI) as a potential game-changer for millions grappling with keratoconus, a disorder that distorts the cornea and threatens sight. This innovation hints at a future where technology could pinpoint exactly who needs urgent intervention, offering a lifeline to preserve vision.
The implications of such a development are profound, especially for younger patients who often face this condition during critical years of education and career building. AI’s promise lies in its ability to analyze vast amounts of data with precision, potentially transforming how eye care specialists approach diagnosis and treatment. This advancement could mark the dawn of a new era, where personalized care becomes the norm rather than the exception.
Understanding Keratoconus and Its Profound Impact
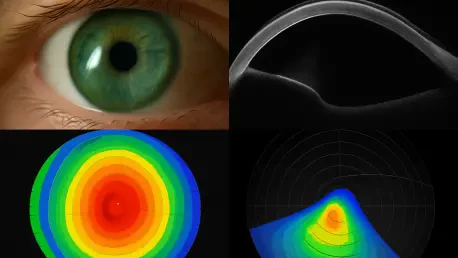
Keratoconus affects about 1 in 350 individuals, typically striking during adolescence or early adulthood, when clear vision is vital for daily life. The condition causes the cornea—the eye’s clear front surface—to thin and bulge into a cone shape, warping vision and sometimes leading to severe impairment. If not addressed early, it often necessitates corneal transplantation, which stands as the leading reason for such surgeries across Western nations, placing a heavy burden on both patients and healthcare systems.
Beyond the physical toll, the emotional and financial strain of managing this condition can be overwhelming. Patients frequently endure years of uncertainty, toggling between corrective lenses and the looming possibility of surgery. The challenge lies in distinguishing between cases that will remain stable and those poised to worsen rapidly, a gap that current diagnostic methods struggle to bridge effectively.
How AI Is Revolutionizing Keratoconus Management
A pioneering study from Moorfields Eye Hospital and University College London, spearheaded by Dr. Shafi Balal, has introduced an AI algorithm capable of predicting keratoconus progression with remarkable accuracy. By scrutinizing over 36,000 corneal images from 6,684 patients via optical coherence tomography (OCT), the technology sorts individuals into low-risk and high-risk categories from their initial consultation. Two-thirds of patients were flagged as low-risk, suitable for routine check-ups, while the remaining third required immediate corneal cross-linking—a procedure effective in halting progression in over 95% of cases.
Remarkably, when data from a follow-up visit was added, the algorithm’s precision climbed to 90%, showcasing its potential to customize treatment plans early on. This capability not only aims to avert vision loss but also reduces the load of unnecessary appointments, allowing resources to be channeled toward those in critical need. Such efficiency could redefine patient care, making interventions both timely and targeted.
Expert Insights on AI’s Transformative Potential
Dr. Balal has hailed this research as a landmark achievement, noting it as the first to deliver such precise predictions of keratoconus progression over a two-year span using imaging and patient data. His enthusiasm reflects the study’s potential to shift clinical paradigms. Echoing this sentiment, Dr. José Luis Güell, a cornea specialist and ESCRS Trustee from Barcelona, who was not part of the study, emphasized the difficulty of timing treatments to prevent escalation to transplants.
Dr. Güell commended the AI’s capacity to identify high-risk patients at the outset, suggesting it could minimize complications and lessen monitoring for stable cases. Both experts share a cautious optimism, stressing that real-world validation is essential to ensure reliability. Their perspectives highlight a collective hope that this technology, if proven effective, could safeguard vision for countless young individuals facing this challenging condition.
Practical Pathways for AI Integration in Eye Care
Implementing AI into clinical settings for keratoconus management involves a series of actionable steps for healthcare providers. Clinics must first invest in compatible imaging tools like OCT to generate the detailed data required for AI analysis. Equipping staff with training to understand and act on AI-generated risk assessments will also be crucial for smooth adoption into daily practice, ensuring that technology complements human expertise.
Additionally, a structured approach to patient care can be established: high-risk individuals should be prioritized for immediate cross-linking, while low-risk patients follow a reduced monitoring schedule, optimizing appointment availability. Ongoing efforts to test and refine the algorithm’s safety across varied populations and imaging systems remain vital, as the research team continues to enhance its accuracy. These measures lay the groundwork for a future where AI not only predicts but also protects vision with unprecedented precision.
Reflecting on a Visionary Leap Forward
Looking back, the strides made in harnessing AI to combat keratoconus stand as a testament to technology’s power in transforming healthcare challenges into solvable puzzles. The journey from uncertainty to targeted treatment illuminated a path where early intervention became a shield against vision loss for many. This breakthrough underscored the value of innovation in addressing long-standing gaps in eye care.
As the field moves forward, the focus shifts to scaling this technology, ensuring its accessibility across diverse regions and healthcare settings. Continued collaboration between researchers, clinicians, and tech developers promises to refine these tools further, potentially extending their reach to other eye conditions. The hope is clear: to build on this foundation, creating a landscape where no patient’s sight is lost to preventable progression.