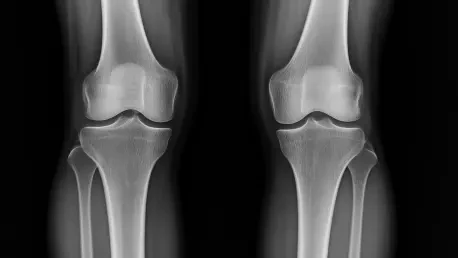
What if a glimpse into the future could save millions from the crippling pain of osteoarthritis, a condition affecting over 500 million people worldwide? Picture a tool that shows how a knee joint might look a year from now, revealing the silent progression of this debilitating disease. This isn’t a distant dream but a reality crafted by cutting-edge artificial intelligence developed at the University of Surrey. This technology, which predicts future knee X-rays with startling accuracy, is poised to redefine how patients and doctors tackle one of the leading causes of disability. Dive into a story of innovation that could transform joint health forever.
Why This Matters for Joint Health
Osteoarthritis stands as a formidable challenge, stripping mobility and independence from countless individuals, particularly older adults. With no known cure, the disease’s unpredictable path makes timely intervention a critical yet elusive goal. The ability to foresee how it might advance in a specific patient could shift the paradigm from reactive treatment to proactive care. This AI breakthrough offers just that—a chance to anticipate deterioration before it becomes debilitating, potentially saving healthcare systems billions while improving quality of life for those affected.
The stakes are high, as the global burden of this condition continues to grow with aging populations. Predictive tools like this one aren’t merely technological novelties; they address a pressing gap in personalized medicine. By providing a window into a patient’s future joint health, this system empowers both clinicians and patients to make informed decisions, highlighting the urgent need for such innovations in chronic disease management.
How AI Sees Tomorrow’s Knees
At the heart of this advancement lies a sophisticated generative diffusion model, a type of AI that crafts realistic future knee X-ray images up to a year ahead. Trained on nearly 50,000 X-rays from almost 5,000 patients—one of the largest datasets of its kind—this system doesn’t just predict; it visualizes. Alongside each image, a risk score quantifies the likelihood of disease progression, offering a dual lens of insight that blends visual and numerical data for a comprehensive outlook.
What sets this tool apart is its efficiency and clarity. It operates nine times faster than comparable models and in a more compact form, making it practical for busy clinical settings. Additionally, the AI pinpoints 16 specific areas on the knee joint in its generated images, showing exactly where changes are expected. This transparency tackles a common flaw in earlier AI systems, which often left doctors guessing about the basis for predictions, paving the way for greater trust in machine-assisted diagnostics.
Expert Perspectives on a Game-Changing Tool
David Butler, study lead at the University of Surrey’s Centre for Vision, Speech and Signal Processing, underscores the emotional impact of this technology. “Visualizing a future state of their knee can be a powerful motivator for patients,” he notes. “It pushes them to commit to therapies or lifestyle changes that might otherwise feel abstract or optional.” His insight reveals how a simple image can bridge the gap between clinical advice and patient action.
Professor Gustavo Carneiro, an AI and machine learning expert involved in the project, focuses on the technical triumph. “This system overcomes past barriers by merging speed, precision, and interpretability,” he explains. “These elements are non-negotiable for real-world medical use.” Early pilot feedback also suggests that such visualizations enable doctors to spot high-risk cases sooner, potentially altering the trajectory of the disease with timely interventions. Together, these voices paint a picture of a tool that resonates on both human and scientific levels.
Real-World Impact Through Visual Clarity
Imagine a patient sitting in a doctor’s office, staring at two X-rays side by side—one showing their knee today, the other a predicted image of next year. This stark comparison can turn vague warnings into tangible urgency, prompting adherence to physical therapy or weight management plans. For many, seeing the potential wear and tear firsthand cuts through denial or procrastination, fostering a proactive mindset that could delay severe outcomes.
Clinicians, too, gain a sharper edge from this visual aid. Instead of relying solely on abstract risk scores or generalized statistics, they can discuss specific areas of concern with patients, tailoring treatment to individual needs. This personalized approach, grounded in concrete imagery, enhances communication during consultations, ensuring that both parties grasp the severity and timeline of potential progression. The result is a collaborative effort toward better joint health, rooted in mutual understanding.
Steps to Bring AI into Everyday Care
Turning this innovation from a research triumph into a clinical staple requires deliberate action. Training healthcare providers to interpret the AI’s outputs—both the predicted images and risk scores—is a crucial first step. Equipping them with the skills to integrate these insights into care plans ensures that the technology enhances rather than complicates their workflow, maximizing its practical value.
Beyond education, partnerships with hospitals and clinics are essential to pilot the system in diverse settings. Gathering real-world data from varied patient groups will refine its accuracy and adaptability, ensuring it serves a broad population effectively. Additionally, exploring applications for other chronic conditions, such as heart disease or lung damage, could expand its impact, adapting the model to different types of medical imaging for wider preventive reach. These steps, already under consideration by the research team, signal a commitment to translating innovation into tangible health benefits.
Looking back, the journey of this AI system reflects a remarkable leap in osteoarthritis care, blending predictive power with human-centric design. As efforts unfold to integrate it into medical practice, the focus remains on actionable progress—training clinicians, forging partnerships, and broadening applications. The potential to not only transform joint health but also inspire similar tools for other chronic ailments offers a hopeful horizon. Continued collaboration between researchers and healthcare providers promises to turn this vision into a lasting reality, ensuring better outcomes for millions.