Imagine a world where chronic wounds, which afflict millions globally and cost healthcare systems billions annually, could heal faster with less pain and fewer complications. Chronic wounds, such as diabetic ulcers and pressure sores, represent a silent epidemic, often lingering for months or even years, causing immense suffering for patients, especially among the elderly and those with underlying conditions. The advent of AI-integrated conductive hydrogel dressings offers a glimpse into a revolutionary solution that could redefine wound management. This FAQ article aims to explore the potential of this cutting-edge technology by addressing critical questions surrounding its functionality, benefits, and challenges. Readers can expect to gain a thorough understanding of how these smart dressings work, their impact on patient care, and the hurdles that remain before widespread adoption.
The significance of tackling chronic wound care cannot be overstated, as traditional methods often fall short in addressing the complex, dynamic nature of healing. By delving into this topic, the goal is to provide clear, actionable insights into how AI and advanced materials are paving the way for personalized medical solutions. This discussion will cover key aspects of the technology, from real-time monitoring to clinical applications, ensuring a comprehensive overview for anyone interested in the future of healthcare innovation.
Key Questions or Key Topics
What Are AI-Integrated Hydrogel Dressings?
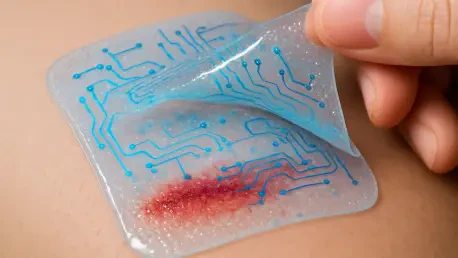
AI-integrated hydrogel dressings are advanced wound care materials designed to monitor and treat chronic wounds using a combination of conductive hydrogels and artificial intelligence. These dressings differ significantly from conventional options by acting as both sensors and therapeutic tools. Their purpose is to provide continuous feedback on wound conditions while actively supporting the healing process, addressing a critical gap in traditional care where static dressings offer no real-time data.
The importance of this innovation lies in its ability to transform wound management from a reactive to a proactive approach. By embedding sensors within biocompatible hydrogels, these dressings can detect changes in temperature, pH, and other vital parameters at the wound site. This data is then analyzed by AI algorithms to guide treatment decisions, offering a level of precision that manual assessments cannot match.
Supporting this concept, the integration of materials like graphene and carbon nanotubes enhances the dressings’ sensitivity and durability, ensuring they remain effective in the challenging environment of a wound. This blend of material science and technology represents a significant step toward personalized healthcare solutions tailored to individual patient needs.
How Do These Dressings Monitor Wound Conditions in Real Time?
Real-time monitoring is a cornerstone of AI hydrogel dressings, enabling healthcare providers to track the status of a wound without invasive procedures. These dressings are equipped with sensors that measure key indicators such as glucose levels, pressure, and even pain signals, providing a comprehensive picture of the wound’s environment. This capability eliminates the need for frequent dressing changes, which can disrupt healing and increase infection risk.
The data collected is transmitted to AI systems for immediate analysis, allowing for timely interventions if issues like infections are detected early. For instance, a sudden change in pH could signal bacterial growth, prompting an adjustment in treatment before the condition worsens. This dynamic feedback loop contrasts sharply with older methods that rely on periodic visual inspections, often missing subtle but critical changes.
Such continuous monitoring not only improves patient outcomes but also reduces the burden on medical staff by automating routine assessments. The technology’s ability to provide actionable insights in real time is a game-changer, particularly for chronic conditions where delays in care can lead to severe complications.
What Role Does Artificial Intelligence Play in Wound Care?
Artificial intelligence serves as the brain behind these smart dressings, processing vast amounts of data to deliver precise, personalized care plans. Machine learning algorithms analyze sensor inputs to predict healing trajectories, identify potential complications, and suggest optimal treatments. With reported accuracy rates reaching up to 96%, this technology offers a level of reliability that surpasses subjective human judgment in many cases.
The significance of AI lies in its capacity to handle complex datasets that would overwhelm manual analysis. For example, by recognizing patterns in physiological signals, it can forecast the risk of infection days before visible symptoms appear, enabling preemptive measures. This predictive power is particularly valuable for chronic wounds, where early intervention can prevent prolonged recovery or even amputation.
Moreover, AI adapts to individual patient profiles over time, refining its recommendations based on ongoing data. This adaptability ensures that treatment remains relevant as the wound evolves, marking a shift toward precision medicine in wound care and setting a new standard for managing persistent health challenges.
How Do These Dressings Actively Promote Healing?
Beyond monitoring, AI hydrogel dressings are engineered to actively support tissue regeneration and combat infection. They possess electroactive properties that stimulate cellular activity at the wound site, encouraging faster recovery. Additionally, built-in mechanisms allow for the controlled release of therapeutic agents, ensuring that medication is delivered precisely where and when it’s needed.
These dressings also exhibit antibacterial effects, reducing the likelihood of complications that often derail healing in chronic wounds. By addressing multiple aspects of care—stimulation, drug delivery, and infection control—within a single platform, they minimize the need for separate treatments, streamlining the process for both patients and providers.
The multifunctionality of these materials highlights their potential to revolutionize care protocols. For conditions like diabetic foot ulcers, where infection and slow healing are constant threats, such integrated solutions could significantly improve outcomes, offering hope to patients who have long struggled with limited options.
What Materials Make These Dressings Effective?
The effectiveness of AI hydrogel dressings hinges on the use of advanced conductive materials such as MXenes, conductive polymers, and graphene. These components are chosen for their biocompatibility, ensuring they interact safely with human tissue, and for their ability to detect subtle physiological changes with high sensitivity. Their durability also allows the dressings to function reliably over extended periods despite the moist, dynamic conditions of a wound.
Material innovation plays a crucial role in customizing these dressings to various wound types and patient needs. For instance, the flexibility of hydrogels ensures they conform to irregular wound shapes, while conductive elements maintain consistent sensor performance. This adaptability is essential for addressing the diverse challenges posed by chronic injuries.
The strategic selection of such materials underscores a broader trend in medical technology toward leveraging cutting-edge science to solve persistent problems. Their integration into wound care products demonstrates a commitment to enhancing both functionality and patient comfort, paving the way for broader applications in healthcare.
What Are the Clinical Applications and Accessibility Benefits?
AI hydrogel dressings hold immense promise for treating a range of chronic conditions, including pressure ulcers and joint wounds, which often require long-term management. Their ability to provide continuous care makes them ideal for use in clinical settings, where precise monitoring can inform treatment decisions. Beyond hospitals, they also support home care by enabling patients to manage their conditions independently while staying connected to healthcare providers through digital platforms.
Accessibility is a key advantage, particularly for individuals in rural or underserved regions where frequent hospital visits are impractical. By facilitating remote monitoring, this technology reduces costs and logistical barriers, ensuring that high-quality care reaches a wider population. This democratization of advanced treatment could reshape how chronic wound care is delivered globally.
The potential to integrate these dressings into everyday healthcare routines further amplifies their impact. As systems evolve to support seamless data sharing between patients and medical teams, the vision of a more connected, efficient care model comes closer to reality, benefiting countless individuals worldwide.
What Challenges Must Be Overcome for Widespread Adoption?
Despite their potential, several obstacles stand in the way of broadly implementing AI hydrogel dressings. Material degradation is a primary concern, as the dressings must maintain functionality in the harsh, wet environment of a wound over time. Ensuring signal stability is equally critical, as inconsistent sensor readings could lead to unreliable AI interpretations and misguided treatments.
Additionally, the generalizability of AI models across diverse patient demographics and wound types remains unproven, requiring extensive real-world testing. Regulatory and logistical hurdles also complicate clinical translation, as standardization and approval processes are necessary to integrate this technology into mainstream healthcare. These barriers highlight the gap between innovation and practical application.
Addressing these challenges demands focused research on improving material resilience, refining algorithms, and establishing partnerships with medical institutions. Overcoming such issues will be essential to unlocking the full transformative power of this technology in chronic wound management.
Summary or Recap
This exploration of AI-integrated hydrogel dressings reveals their potential to redefine chronic wound care through real-time monitoring, intelligent data analysis, and active healing properties. Key takeaways include their ability to provide continuous feedback on wound conditions, predict complications with high accuracy, and deliver targeted treatments using advanced materials. The technology also promises to enhance accessibility by supporting remote and home-based care, addressing systemic healthcare challenges.
The implications of these advancements extend to improved patient outcomes, reduced costs, and a shift toward personalized medicine. Each aspect discussed—from material innovation to clinical applications—underscores a broader movement in healthcare toward data-driven solutions. For those eager to dive deeper, exploring resources on biomaterials and AI in medicine can provide further insight into this evolving field.
Conclusion or Final Thoughts
Reflecting on the journey through this topic, it becomes evident that AI hydrogel dressings mark a turning point in how chronic wounds are managed, offering solutions that were once unimaginable. The fusion of smart materials and artificial intelligence opens doors to faster healing and fewer complications for countless patients who have endured prolonged suffering.
Looking ahead, the focus should shift to actionable steps such as accelerating research into material durability and algorithm optimization to ensure reliability across diverse settings. Collaborative efforts between researchers, healthcare providers, and regulatory bodies are needed to navigate the path to widespread adoption, ensuring that this innovation reaches those in greatest need. Ultimately, considering how such technology could integrate into everyday healthcare routines encourages a broader reflection on embracing advancements that prioritize patient well-being.