Imagine a scenario where a patient, battling cancer that has spread to the brain, undergoes complex treatments like radiation or chemotherapy, only to face uncertainty when follow-up scans can’t clearly show whether the tumor is growing or if the changes are just treatment side effects. This diagnostic dilemma is all too common in managing brain metastases, a devastating complication affecting many with solid tumors such as lung or breast cancer. The stakes are incredibly high—misdiagnosis can lead to unnecessary surgeries or delayed critical care, impacting survival and quality of life. Enter 18F-Fluciclovine PET/MRI, an imaging innovation originally developed for prostate cancer, now showing promise in distinguishing true tumor progression from treatment-related changes in the brain. With early research revealing a remarkable 91% accuracy rate, this tool could redefine precision in neuro-oncology. This article explores the challenges of current methods, the science behind this tracer, its performance in real-world cases, and what lies ahead for its integration into clinical practice, shedding light on a potential breakthrough for patients and clinicians alike.
Understanding the Challenge of Brain Metastases Diagnosis
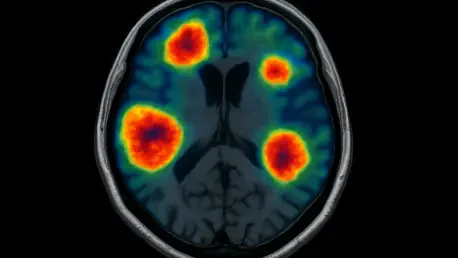
The Limitations of Conventional MRI
Conventional MRI scans, long considered the standard for imaging brain tumors, frequently leave clinicians in a frustrating gray area when trying to determine if changes in the brain signal tumor regrowth or merely reflect side effects like radiation necrosis or inflammation from therapy. This lack of clarity often results in critical errors, such as pursuing invasive procedures that aren’t needed or failing to address actual disease advancement. The overlap in how progression and treatment effects appear on these scans creates a diagnostic blind spot that can jeopardize patient outcomes. 18F-Fluciclovine PET/MRI emerges as a potential solution, leveraging a specialized tracer to highlight active tumor tissue with greater contrast against normal brain matter. By offering a clearer picture, this method aims to reduce the guesswork that plagues conventional imaging, potentially guiding more accurate treatment decisions in complex cases of brain metastases.
Beyond the technical shortcomings of MRI, the broader impact of diagnostic uncertainty reverberates through the healthcare system, affecting not just individual patients but also the efficiency of oncology workflows. When scans are inconclusive, additional testing or invasive biopsies often become necessary, increasing costs and patient stress while delaying definitive care. For those with brain metastases, where time is often critical, these delays can mean the difference between manageable disease and irreversible progression. The introduction of 18F-Fluciclovine PET/MRI into this landscape represents a shift toward precision diagnostics, aiming to cut through ambiguity with data-driven insights. Research into this imaging approach, highlighted at a major neuro-oncology conference, suggests it could significantly outperform traditional methods, providing a lifeline for accurate assessment in post-treatment scenarios.
Why Accurate Detection Matters
The consequences of misdiagnosing brain metastases progression are profound, as an incorrect assessment can lead to treatments that are either overly aggressive or insufficient, both of which carry serious risks for patients already burdened by cancer. Unnecessary surgeries might expose individuals to complications without addressing the actual issue, while missing true progression can allow the disease to advance unchecked, reducing the window for effective intervention. Brain metastases, common in cancers like lung, breast, and melanoma, affect a substantial number of patients, making the need for reliable diagnostics urgent. The emotional and physical toll of uncertainty only compounds the challenge, as patients and families await clarity on the next steps. 18F-Fluciclovine PET/MRI offers hope by targeting active tumor cells with high specificity, potentially minimizing these diagnostic pitfalls and ensuring that clinical decisions align with the true state of the disease.
Moreover, accurate detection extends beyond individual patient care to influence broader trends in oncology, where personalized medicine is increasingly prioritized. When clinicians can confidently distinguish between treatment effects and tumor growth, they can tailor therapies more effectively, avoiding the one-size-fits-all approaches that often fail to account for unique post-treatment responses. This precision is especially critical in brain metastases, where the brain’s delicate environment amplifies the impact of any misstep. The research into 18F-Fluciclovine underscores a growing recognition that advanced imaging is not just a luxury but a necessity in modern cancer management. By reducing the likelihood of misdiagnosis, this technology could pave the way for more streamlined care pathways, ultimately improving survival rates and quality of life for those grappling with this challenging condition.
How 18F-Fluciclovine PET/MRI Works
The Science Behind the Tracer
18F-Fluciclovine, an amino acid-based imaging agent initially approved by the FDA for detecting recurrent prostate cancer, operates on a unique principle that makes it particularly suited for identifying active tumor tissue in the brain during PET/MRI scans. Tumor cells, which often have a heightened uptake of amino acids due to rapid growth, absorb this tracer at a higher rate than surrounding healthy brain tissue, creating a stark contrast visible on imaging. This high tumor-to-brain contrast is a key advantage over conventional methods, allowing for more precise identification of disease progression even after treatments like radiation or immunotherapy that can obscure standard scans. The adaptation of this agent for brain metastases marks an innovative repurposing of existing technology, driven by the urgent need for better diagnostic tools in neuro-oncology, where distinguishing true recurrence from treatment effects remains a persistent challenge.
The mechanism of 18F-Fluciclovine also ties into broader advancements in molecular imaging, reflecting a shift toward targeting specific biological processes rather than relying solely on structural changes seen in traditional MRI. By focusing on metabolic activity, this tracer can reveal the presence of active cancer cells that might otherwise be masked by inflammation or scarring from prior therapies. This capability is particularly valuable in the context of brain metastases, where the complexity of post-treatment changes often confounds diagnosis. The research surrounding this agent, presented at a prominent neuro-oncology meeting, highlights its potential to fill a critical gap in current imaging practices. As studies continue, the scientific community is keenly observing whether this tracer can maintain its promising performance across varied patient profiles and treatment histories, potentially setting a new standard for diagnostic precision.
Study Design and Patient Insights
The ongoing clinical trial evaluating 18F-Fluciclovine PET/MRI targets a specific group of patients with brain metastases from solid tumors, whose prior MRI results left uncertainty about whether observed changes indicated progression or treatment effects. With a goal of enrolling 30 participants, the study has so far analyzed a diverse cohort, including individuals with primary cancers such as lung, breast, and melanoma, all of whom have undergone multimodal therapies like radiation and systemic treatments. The methodology involves measuring the tracer’s uptake through a standardized uptake value maximum (SUVmax), with a cutoff of 4.8 used to differentiate between tumor growth and treatment-related changes. This structured approach ensures that findings are grounded in quantifiable data, providing a robust framework for assessing the tool’s diagnostic potential in real-world clinical scenarios.
Diving deeper into the patient demographics, the trial reflects the varied landscape of cancer care, capturing a mix of tumor types and treatment histories that mirror the challenges faced in everyday oncology practice. Most participants are male, and their primary cancers span common sources of brain metastases, ensuring that the results have broad relevance. The protocol includes initial MRI confirmation of metastases, followed by therapies and regular follow-up scans, with 18F-Fluciclovine PET/MRI introduced when ambiguity arises. Validation of imaging outcomes through surgical resection or extended clinical follow-up adds a layer of rigor to the findings. This diversity and methodological thoroughness underscore the study’s aim to not only test the tracer’s efficacy but also to understand how it performs across different contexts, laying the groundwork for potential widespread adoption if results hold up in larger cohorts.
Performance and Real-World Impact
Impressive Diagnostic Metrics
The performance of 18F-Fluciclovine PET/MRI in distinguishing brain metastases progression from treatment effects stands out with a reported accuracy of 91%, a figure that suggests a significant leap over traditional imaging methods. Equally striking is its 100% sensitivity, meaning it successfully identified every instance of true progression in the studied cases, a critical factor in ensuring no patient misses timely intervention. The perfect negative predictive value further reinforces this reliability, indicating no false negatives were recorded, while a specificity of 89% shows a strong ability to rule out progression when it isn’t present. However, a positive predictive value of 67% points to a moderate rate of false positives, an area where refinement is needed. These metrics, derived from a detailed analysis of patient scans, highlight the tracer’s potential to transform diagnostic confidence in neuro-oncology.
Beyond the numbers, these diagnostic metrics carry profound implications for clinical decision-making, where the cost of error can be extraordinarily high in brain metastases management. The ability to avoid missing progression cases addresses one of the most pressing fears in oncology—delayed treatment that allows disease to advance unchecked. While the presence of some false positives suggests caution in interpreting positive results, the overall balance of sensitivity and accuracy positions 18F-Fluciclovine PET/MRI as a tool that could reduce unnecessary interventions compared to less specific methods. As the trial progresses toward its full enrollment, these early statistics provide a compelling case for further investment in this technology, potentially reshaping how post-treatment surveillance is conducted for patients with brain metastases across various cancer types.
Case Studies: Successes and Setbacks
Examining real patient outcomes from the study brings the data on 18F-Fluciclovine PET/MRI to life, illustrating its practical strengths in identifying brain metastases progression. One notable case involved a patient with a breast cancer primary tumor, where a treated brain lesion showed a significantly elevated SUVmax of 13 on the scan. This result prompted a classification of progression, which was later confirmed through surgical resection and pathological analysis as recurrent carcinoma, validating the tracer’s accuracy in a high-stakes scenario. Such successes underscore the potential of this imaging method to guide critical treatment decisions with precision, ensuring that patients receive appropriate care when tumor growth is genuinely present, and offering a level of certainty that standard MRI often cannot match in post-treatment evaluations.
However, not all cases yielded perfect results, revealing the complexities of applying 18F-Fluciclovine PET/MRI across diverse clinical contexts. In another instance, a patient with melanoma exhibited an SUVmax of 9.0, leading to an initial diagnosis of progression, but subsequent surgical findings identified the change as treatment-related rather than tumor growth. Researchers hypothesized that active immunotherapy might have influenced the tracer uptake, resulting in a false positive. This setback highlights that external factors, such as ongoing therapies or specific tumor characteristics, can occasionally skew results, necessitating a nuanced interpretation of scans. These contrasting cases emphasize the importance of continued research to refine diagnostic criteria and account for variables that might affect the tracer’s performance in real-world applications.
Looking Ahead: Challenges and Potential
Overcoming Study Hurdles
Despite the encouraging early results of 18F-Fluciclovine PET/MRI in brain metastases diagnosis, the research faces significant challenges that must be addressed to solidify its place in clinical practice. Patient recruitment has proven difficult due to strict eligibility criteria, slowing the trial’s progress toward its target of 30 participants and limiting the breadth of data available for analysis. Additionally, the presence of rare false positives and negatives suggests that factors like tumor type, individual patient responses, or concurrent therapies might influence outcomes in unexpected ways. Researchers emphasize the need for larger, more diverse cohorts to better characterize the tracer’s performance and establish more reliable diagnostic thresholds. Tackling these hurdles is essential to ensure that this promising tool can be trusted across varied clinical settings without risking misdiagnosis.
Another layer of complexity lies in optimizing the integration of this imaging technique into existing medical workflows, where logistical and cost considerations often play a role in adoption. Expanding the study to include a wider range of patients and treatment scenarios will help uncover any hidden limitations, such as specific cancers or therapies that might consistently affect results. The commitment to refining SUVmax cutoffs and other diagnostic parameters reflects a dedication to precision, but it also underscores the reality that this technology is still in a developmental phase. Overcoming these obstacles through rigorous research and collaboration across institutions could pave the way for 18F-Fluciclovine PET/MRI to become a cornerstone of brain metastases management, offering clarity where traditional imaging falls short and addressing a critical unmet need in oncology.
Future Horizons in Neuro-Oncology Imaging
Looking to the future, the implications of 18F-Fluciclovine PET/MRI extend far beyond the current trial, pointing toward a potential transformation in how brain metastases are monitored and managed in clinical settings. The high sensitivity and negative predictive value demonstrated so far suggest that this tool could prevent missed progressions, a crucial step in improving patient outcomes through timely interventions. However, the moderate rate of false positives indicates a need for complementary diagnostics or adjusted protocols to enhance overall accuracy. As the first major study to explore this tracer in the context of brain tumors, it sets a precedent for expanding amino acid-based PET imaging into new areas, potentially broadening its applications and influencing guideline development for post-treatment surveillance in neuro-oncology.
Furthermore, the trajectory of this research aligns with a larger movement toward precision diagnostics, where tailored imaging solutions are increasingly seen as vital to effective cancer care. Future efforts should prioritize validating these findings in larger populations and investigating how specific treatments impact tracer performance to minimize diagnostic errors. Establishing standardized protocols for clinical use will also be key to ensuring consistency across different healthcare environments. If successful, 18F-Fluciclovine PET/MRI could redefine the standard of care for brain metastases, reducing uncertainty and enabling more personalized treatment plans. The path forward involves not just overcoming current limitations but also anticipating how this technology might evolve alongside other innovations, ultimately shaping a future where diagnostic precision is the norm rather than the exception in tackling complex cancers.