Every three minutes somewhere in the world, a person with type 1 diabetes calculates a dose of insulin and still lives with the nagging reality that even perfect math will not reproduce the split-second precision of native β-cells. Clinicians point to the autoimmune destruction that erased those cells in the first place, leaving management dependent on pumps and sensors that reduce—but do not eliminate—danger. Transplant specialists add that islet infusions proved a point: restored β-cell mass can normalize glycemia, yet the roadblock of immunosuppression and scarce donors keeps that solution out of reach for most.
Immunologists and engineers converge on the same urgency: physiologic glucose control is the difference between a stable life and a slow accrual of complications, but systemic drugs and limited organs cannot scale. Device developers argue that immune-shielded cells shift the stakes by removing the need for lifelong immunosuppression, while health economists warn that durability and manufacturability must be built in from the start. What rises from these views is a shared premise that replacement without immune design is a trap.
As a roadmap, researchers describe a dual track—nudge the adult pancreas to regenerate new β-cells and bring in stem cell–derived replacements—then surround both with local, built-in immune protection. Developmental biologists emphasize that this only works if derived cells mature to adult-like function, while regulators underline that safety switches and product consistency are not add-ons but gatekeepers.
Designing a curative platform: rebuilding β-cell mass and defusing autoimmunity in tandem
Roundtable discussions consistently frame regeneration and immune control as inseparable halves of the same therapy. Transplant surgeons highlight that recurrent autoimmunity can erase even flawless grafts, whereas immunologists caution that broad suppression trades one risk for another. The compromise they endorse is targeted tolerance at the graft site, with systemic exposure kept minimal.
Manufacturing leaders add a hard practical edge: scalable cell supply, stable potency, and predefined release criteria are the levers that determine who actually receives therapy. Ethicists and payers echo that equitable access hinges on predictable, high-yield processes, pushing the field toward unified platforms rather than bespoke, one-off solutions.
Unlocking in situ regeneration in the adult pancreas
Gastroenterologists and developmental biologists debate whether the adult pancreas hides true progenitors or merely toggles stressed cells into plastic states. Single-cell data, they note, reveal ductal and acinar cells with progenitor-like signatures after injury, hinting at neogenesis beyond the limited replication seen in adult β-cells. Endocrinologists counter that dedifferentiation can blunt insulin secretion, so regeneration must avoid creating fragile intermediates.
Methodologists agree on a common toolkit: transient NGN3 reactivation to re-open endocrine competence, careful tuning of Notch and Wnt/β-catenin to expand precursors, and relief of Hippo signaling to activate YAP where needed. In preclinical models, those levers yielded β-like cells with glucose responsiveness, albeit variably. The safety camp stresses that systemic pathway modulation is risky; precision delivery and on–off control are the only acceptable routes.
Across these views runs a cautionary thread: miscalibrated cues can produce dysfunctional cells or off-target growth. As a result, drug developers favor localized depots or vector systems with restricted tropism, while trialists propose staged dose escalation with functional monitoring through multi-omic biomarkers rather than single readouts.
Renewable β-cells from pluripotent platforms move into patients
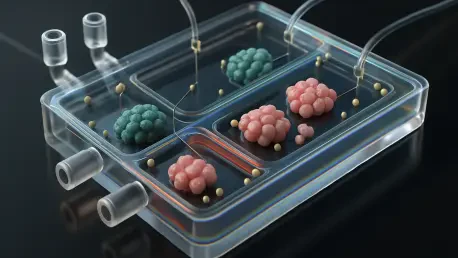
Clinical investigators point to early human signals from Vertex and ViaCyte—endogenous insulin production, measurable C-peptide, and reductions in exogenous insulin—as validation that pluripotent platforms can cross the translational gap. Device specialists explain that macro- and microdevices help deliver and protect these cells, though each approach presents trade-offs in retrieval, vascularization, and nutrient diffusion.
Manufacturing experts press on batch fidelity, adult-like maturation, and tumor safeguards as the core triad of reliability. Quality leaders advocate multi-omic release criteria that correlate with dynamic glucose-stimulated insulin secretion, while safety teams champion suicide switches and depletion of residual pluripotent cells. Health system stakeholders weigh allogeneic products—efficient but facing allo- and autoimmunity—against autologous iPSCs—customized yet costly and not inherently protected from autoimmune relapse.
Policy analysts and payers warn that logistics and price could blunt impact if not engineered out early. Meanwhile, gene-editing proponents see an opening to harmonize allogeneic supply with immune evasion, provided edits remain minimal, validated, and trackable over time.
Building the immune moat: making β-cells and their niche invisible yet safe
Biomaterials researchers argue for local tolerance as the lead defense, focusing on encapsulation mechanics, anti-fibrotic coatings, and oxygen support to prevent the slow suffocation that dooms grafts. Surgeons remind the field that devices must integrate with host vasculature without triggering foreign body responses; otherwise, protection becomes isolation, and isolation becomes failure.
Gene editors propose “stealth” cells by modulating HLA and upregulating PD-L1, while immune therapists champion antigen-specific tolerance via vaccines, engineered Tregs, or tolerogenic dendritic cells. Comparative discussions land on combination regimens: a modest stealth profile plus local immunoregulatory cues like IL-10 often looks safer than heavy edits or broad immunosuppression alone. Regulators across regions differ on device pathways and gene-editing oversight, so program strategies increasingly adapt to the strictest common denominator.
Industry strategists note that adoption will track clarity: well-defined product–device combinations, transparent risk mitigation, and real-world monitoring plans. Without that alignment, even strong clinical data may stall in committee rooms rather than reaching clinics.
Lessons from α-cells and systems cues that calibrate true physiologic control
Endocrinologists often point to α-cells as the islet’s tough survivor—less visible to autoimmunity, more resistant to cytokine stress, and equipped with anti-apoptotic programs. That profile inspires β-cell engineering: dialing down autoantigen display, incorporating survival pathways, and shaping the niche with anti-inflammatory signals to mimic α-cell resilience without blunting function.
Reprogramming specialists outline α-to-β transdifferentiation as a flexible reserve, yet emphasize preserving counterregulation to avoid dangerous hypoglycemia. They highlight modulators such as GLP-1 for survival and plasticity and GDF11 for rejuvenation of regenerative capacity. The consensus is pragmatic: transdifferentiation should complement, not replace, β-cell replacement and needs guardrails to maintain glucagon competence.
Systems biologists push the conversation beyond C-peptide, urging attention to neuroendocrine wiring, circadian entrainment, and organ-on-chip maturation that simulates real-life flux. Their stance is that true physiologic control demands fast kinetics, appropriate suppression during fasting, and poised counterregulation—benchmarks that require integrated testing, not single snapshots.
What to do now: an integration playbook for durable, scalable therapies
Program leaders distilled a core insight: β-cell replacement must launch hand-in-hand with targeted immune protection and rigorous maturation standards. Without that triad, gains fade or safety risks rise. Trial designers therefore prioritize adult-like functionality, context-aware biomarkers, and predefined fail-safes to keep outcomes transparent and reversible if needed.
Operationally, experts recommend embedding multi-omic release criteria into GMP workflows, pairing cells with local tolerance layers such as PD-L1 or IL-10 microenvironments, and including safety switches at the construct level. They also urge staged trials that separate tumorigenicity risk from efficacy readouts, with fibrosis-resistant devices that provide oxygen support during the vulnerable engraftment window.
Technologists add that modular, minimal gene edits reduce off-target risk and ease regulatory review, while AI-guided analytics can match patients to product–device combinations and dosing schemes based on immune profiles and glycemic variability. Across these steps, the shared aim is durable control that scales beyond pilot cohorts and proves sustainable in day-to-day care.
The path forward: coordinated biology and engineering to outpace autoimmunity
This roundup closed by synthesizing a throughline: regeneration and immune design moved in parallel, guided by developmental control and lessons from α-cell resilience. Durability, manufacturability, and cost functioned as gatekeepers of real-world impact, while evolving pathways for gene-edited and device-enabled products shaped deployment timelines and study architecture. Suggested further reading included clinical protocol summaries, regulatory guidances on combination products, manufacturing playbooks for pluripotent platforms, and consensus statements on antigen-specific tolerance.