Could a single injection harness the body’s own healing power to mend a torn ligament or damaged cartilage, slashing recovery time for athletes and active individuals? This isn’t a distant dream but a reality unfolding through Bone Marrow Aspirate Concentrate (BMAC) therapy, a groundbreaking approach in orthopedic care that is capturing attention across clinics and research labs for its potential to transform how joint injuries are managed by offering a less invasive path to recovery. Dive into the story of BMAC and explore how it’s rewriting the rules of healing.
Why BMAC Is a Game-Changer in Joint Recovery
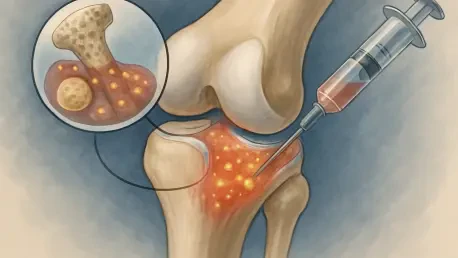
Joint injuries, from torn anterior cruciate ligaments (ACL) to meniscus damage, sideline millions each year, disrupting lives with pain and prolonged downtime. Traditional solutions often rely on surgery paired with grueling rehabilitation, yet full recovery remains elusive for many. BMAC therapy emerges as a beacon of hope, tapping into the body’s innate repair systems by using concentrated bone marrow to accelerate healing and reduce inflammation at the injury site.
This innovative treatment isn’t just another medical trend; it’s a shift toward regenerative medicine that prioritizes the body’s natural abilities over invasive procedures. By delivering stem cells and growth factors directly to damaged tissues, BMAC offers a promising alternative or complement to surgery. Its growing adoption in sports medicine and orthopedics signals a turning point, addressing the urgent need for faster, more effective recovery options in a world where joint health is paramount.
The Heavy Toll of Joint Injuries and Regenerative Hope
The impact of joint injuries extends far beyond the initial pain, often leading to chronic issues or even permanent limitations. Conditions like ACL or medial collateral ligament (MCL) tears affect not only professional athletes but also everyday individuals, with over 2 million cases reported annually worldwide. Standard treatments, while sometimes necessary, carry risks of complications and don’t always restore pre-injury function, leaving patients searching for better answers.
BMAC therapy steps into this gap with a regenerative approach that could redefine recovery standards. Extracted from a patient’s own bone marrow, typically from the hip’s iliac crest, the concentrate is rich in healing components that stimulate tissue repair. This method holds particular promise for reducing reliance on extensive surgical interventions, presenting a less disruptive path that aligns with the growing demand for personalized, minimally invasive care.
How BMAC Works to Mend Joints
At its core, BMAC therapy involves a straightforward yet powerful process: bone marrow is drawn from a patient, often from the hip, and processed to isolate a high concentration of stem cells and growth factors. This potent mixture is then injected into the injured joint—be it a torn ligament or damaged cartilage—either as a standalone treatment or alongside surgical repair. The goal is to jumpstart regeneration and curb inflammation directly at the source of injury.
The effectiveness of this therapy, however, hinges on subtle variables. Research indicates that the composition of bone marrow can differ based on the extraction site, with hip marrow often boasting a higher stem cell count compared to other areas like the shoulder. These variations can influence healing outcomes, underscoring the importance of precision in how BMAC is prepared and applied to ensure optimal results for each patient.
Cutting-Edge Insights from Colin Herna’s Research
In the labs of Lehigh University, doctoral student Colin Herna is unraveling the intricate details of BMAC’s potential. Leading a study published in ACS Omega, Herna and his team analyzed 109 unique proteins from bone marrow samples taken from both hip and shoulder sites, identifying six proteins with distinct concentration differences. “These variations aren’t trivial—they could shape how effectively a patient heals based on the marrow’s origin,” Herna explains.
This research leverages machine learning models to dissect BMAC composition, revealing how the microenvironment of different bones affects therapeutic outcomes. A critical takeaway from Herna’s work is the current lack of standardization in BMAC preparation, which can lead to inconsistent results across treatments. His findings lay the groundwork for refining this therapy, pushing the field toward more reliable and tailored applications starting from 2025 onward.
Personalizing BMAC for Optimal Joint Healing
Tailoring BMAC therapy to individual needs is the next frontier in maximizing its impact. The choice of extraction site—whether hip for lower body injuries like knee damage or shoulder for upper body issues like rotator cuff tears—can play a pivotal role in treatment success. Patients and clinicians must weigh these options based on injury location and the specific healing components required for optimal recovery.
Beyond site selection, transparency in treatment protocols is essential. Variations in how marrow is extracted and concentrated can affect the therapy’s potency, making it vital for providers to adopt consistent methods. Emerging tools, such as Herna’s machine learning framework, hold promise for customizing BMAC by factoring in patient-specific traits like age or activity level, steering regenerative medicine closer to a truly individualized approach.
Reflecting on BMAC’s Journey and Next Steps
Looking back, BMAC therapy has carved a remarkable path in reshaping joint injury treatment, offering a glimpse of healing powered by the body’s own resources. Studies and clinical applications have demonstrated its capacity to mend tissues like torn ligaments with reduced invasiveness, while researchers like Colin Herna have illuminated the nuances of marrow composition. The integration of data-driven tools has marked a significant stride in understanding how to optimize this regenerative approach.
Moving forward, the focus must shift to standardization, ensuring that every patient receives consistent, high-quality treatment regardless of where or how BMAC is prepared. Clinicians are encouraged to adopt emerging research insights, tailoring extraction sites and methods to match specific injuries. As the medical community continues to refine this therapy, patients stand to gain from a future where joint recovery is not just faster, but uniquely suited to their needs, heralding a new era of personalized care.