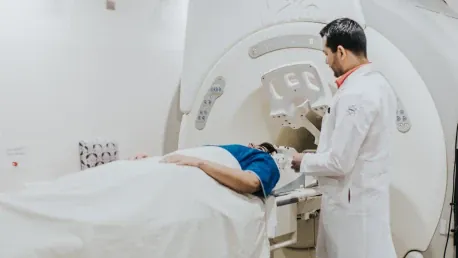
Harnessing the power of artificial intelligence (AI), researchers have unlocked the potential of whole-body magnetic resonance imaging (MRI) to predict health risks, paving the way for smarter, personalized prevention strategies. This breakthrough is highlighted in a recent study published in the journal eBioMedicine. Researchers from Germany and the United States developed and validated a deep learning framework for automated volumetric body composition analysis from whole-body MRI and assessed its prognostic value for predicting all-cause mortality in a large Western population. This development could revolutionize how medical professionals evaluate and manage patients’ health by providing precise and individual risk assessments.
Background and Importance of Body Composition Analysis
The analysis of body composition, which includes metrics such as adipose tissue compartments and skeletal muscle, has shown significant associations with clinical outcomes, marking them as vital imaging biomarkers for personalized risk assessment. Researchers have long known that detailed body composition analysis can provide critical insights into an individual’s health status and potential future risks. However, the routine quantification of these measures from imaging modalities like MRI is limited in clinical workflows due to the high time and resource demands.
MRI, with its superior capability to differentiate tissue types and assess their distribution, offers substantial potential for comprehensive body composition analysis. Manual quantification of body composition through MRI is labor-intensive. Automated approaches, however, have the potential to overcome these barriers. AI-driven volumetric analysis presents an opportunity to overcome current limitations, allowing for more accurate and scalable assessments. This advancement highlights the necessity of developing standardized tools to ensure clinical applicability across diverse populations. The ability to automatically and accurately quantify body composition can lead to better predictive models and more effective health intervention strategies tailored to individual patient needs.
Study Design and Methodology
This study utilized data from two extensive population-based cohort studies: the UK Biobank (UKBB), involving participants aged 45-84 years, and the German National Cohort (NAKO), with participants aged 40-75 years. Comprehensive clinical data were collected from both studies, which employed a detailed MRI protocol, including axial whole-body T1-weighted Three-Dimensional Volumetric Interpolated Breath-hold Examination (3D VIBE) Dixon sequences, used for body composition analysis. Ethical approvals were obtained, and informed consent was secured from all participants. The primary aim was to develop a deep learning framework for automated quantification of volumetric body composition measures, such as subcutaneous adipose tissue (SAT), visceral adipose tissue (VAT), skeletal muscle (SM), skeletal muscle fat fraction (SMFF), and intramuscular adipose tissue (IMAT). This was done using whole-body MRI.
The framework’s performance was evaluated primarily within the UKBB cohort, focusing on its prognostic value in predicting all-cause mortality. Researchers also aimed to assess correlations between whole-body volumetric measures and traditional single-slice body composition estimation at the L3 vertebra. The deep learning model used Dixon sequence imaging inputs to generate segmentation masks, enabling the quantification of both volumetric and single-slice body composition. Experienced radiologists performed manual annotations for model training, which were then independently validated. Statistical analyses included survival modeling and correlation assessments, using harmonized datasets to minimize distributional differences. This rigorous study design ensures that the findings are robust and applicable to real-world clinical settings, potentially transforming medical imaging practices.
Key Findings and Statistical Analysis
The UKBB cohort included 36,317 participants (18,777 females and 17,540 males), with a mean age of 65.1 ± 7.8 years and a mean body mass index (BMI) of 25.9 ± 4.3 kg/m². Analysis of body composition revealed higher volumetric subcutaneous adipose tissue (VSAT), skeletal muscle fat fraction (VSMFF), and intramuscular adipose tissue (VIMAT) in females. Meanwhile, males exhibited greater visceral adipose tissue (VVAT) and skeletal muscle volume (VSM) (all p
Over a median follow-up period of 4.77 years in the UKBB, 634 deaths (1.7%) were recorded. Kaplan-Meier survival curves demonstrated that participants in the lowest 10th percentile of VSM and the highest 10th percentiles of VSMFF and VIMAT exhibited significantly higher mortality rates (log-rank p
Comparison with Traditional Methods
Single-slice area measures at the L3 vertebra yielded consistent results, with lower skeletal muscle area (ASM) and higher fat fraction (ASMFF) and intramuscular adipose tissue (AIMAT) being associated with mortality. However, these associations weakened for ASM and AIMAT after full adjustment. Reclassification analyses demonstrated that volumetric measures were more effective at identifying high-risk individuals than single-slice measures, evidenced by significant net reclassification improvement for skeletal muscle (NRI = 0.053, 95% CI [0.016–0.089]). Correlation analysis between volumetric whole-body and single-slice measures showed strong concordance at specific vertebral levels, such as L3 for VAT (R = 0.892) and SM (R = 0.944).
The findings were replicated in the NAKO cohort, though correlation varied significantly by BMI and sex strata. The deep learning framework demonstrated high accuracy, with Dice coefficients exceeding 0.86 and strong agreement between manual and automated segmentation results (r > 0.97). These results highlight the superior performance of AI-driven volumetric analysis over traditional methods, making it a more reliable tool for predicting health outcomes. Furthermore, the study emphasized the need for personalized analysis based on sex and BMI variations, as these factors significantly influence body composition metrics and their prognostic value.
Conclusions
Harnessing the power of artificial intelligence (AI), researchers have unlocked the potential of whole-body magnetic resonance imaging (MRI) to predict health risks, paving the way for smarter, personalized prevention strategies. This breakthrough was highlighted in a recent study published in the journal eBioMedicine. Researchers from Germany and the United States developed and validated a deep learning framework designed for automated volumetric body composition analysis from whole-body MRI scans. They then assessed its prognostic value for predicting all-cause mortality in a large Western population. By offering precise and individualized risk assessments, this innovation stands to revolutionize how medical professionals evaluate and manage patients’ health. Such advancements could lead to more tailored treatment plans and early interventions, ultimately improving patient outcomes and setting new standards in the medical field.