A transformative artificial intelligence tool promises to redefine cardiac care by enabling a standard imaging technique to see what was previously invisible: the specific arterial plaques most likely to cause a catastrophic heart attack. Researchers at the Korea Advanced Institute of Science and Technology (KAIST) developed this breakthrough method, which enhances optical coherence tomography (OCT) to provide a biochemical map of coronary arteries. This addresses a critical limitation in current diagnostics and offers a powerful new way to predict risk and prevent sudden cardiac events before they happen. By unlocking latent information within existing technology, this software-based innovation stands to make proactive, personalized cardiology more accessible and effective, potentially saving countless lives by identifying hidden dangers lurking within the walls of a patient’s arteries.
The Innovation: Seeing the Unseen in Coronary Arteries
Bridging a Critical Diagnostic Gap
The fundamental challenge this research overcomes is the inherent limitation of conventional optical coherence tomography in assessing the chemical composition of arterial plaque. While standard OCT excels at producing detailed, high-resolution structural images of the interior of blood vessels, it fundamentally lacks the ability to reliably differentiate between stable, fibrous plaques and their highly dangerous, lipid-rich counterparts. These unstable, fatty deposits are extremely susceptible to rupture, an event that acts as the primary trigger for the majority of heart attacks and other acute coronary syndromes. This significant diagnostic blind spot has long hindered the ability of cardiologists to accurately evaluate a patient’s immediate risk profile and make optimally informed decisions during critical interventions, such as angioplasty and stent placement. This gap in knowledge means that clinicians often have to make crucial treatment choices without a complete picture of the plaque’s true vulnerability.
The newly developed AI-driven method is designed specifically to close this informational divide by leveraging data that is already captured by OCT systems but has remained underutilized until now. It functions as a sophisticated computational upgrade rather than a new piece of hardware, ingeniously unlocking hidden spectral information contained within the standard OCT signal. This innovative approach allows physicians to non-invasively characterize the biochemical makeup of the artery wall in real time, providing an unprecedentedly clear and objective view of plaque composition. By distinguishing high-risk lipid pools from benign tissue, the technology furnishes cardiologists with the crucial insights needed to more accurately assess plaque vulnerability, thereby personalizing treatment strategies and enhancing patient safety without requiring hospitals to invest in new, specialized, and costly imaging equipment. This software-based solution seamlessly integrates with the existing clinical workflow, promising a rapid and widespread adoption.
The Power of AI-Enhanced Imaging
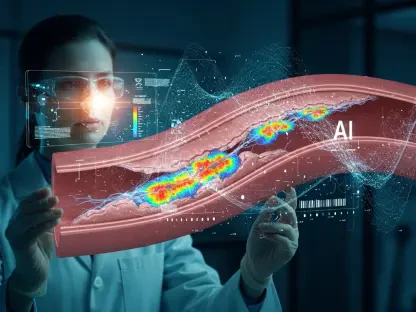
The technology’s methodology is rooted in the principles of spectroscopic analysis, extracting subtle, wavelength-dependent optical properties from the raw OCT data stream. It capitalizes on the fact that different biological tissues—including lipids, fibrous material, and calcium deposits—interact with light in distinct and measurable ways across the light spectrum. The research team developed a powerful deep learning model trained specifically to recognize the unique spectral signatures associated with lipid-rich deposits, which are otherwise imperceptible in a standard OCT image. By completely automating this highly complex task of pattern recognition, the AI system can objectively and quantitatively generate a detailed map showing the precise distribution of dangerous lipids throughout the vessel wall. This provides a far more comprehensive and actionable assessment than was previously possible, transforming the qualitative images of OCT into a quantitative diagnostic tool for risk stratification.
A pivotal advantage of this artificial intelligence model is its reliance on a “weakly supervised learning” framework, a design choice that significantly accelerates its development and deployment. Traditionally, training AI models for medical imaging is a notoriously laborious process, requiring clinical experts to spend countless hours manually outlining and annotating specific features on a pixel-by-pixel basis across thousands of images. This process is not only time-consuming but also prone to subjective variability. The KAIST team ingeniously circumvented this bottleneck by training their system using much simpler, frame-level labels that only indicate the presence or absence of lipids within an entire image frame. This streamlined approach drastically reduces the annotation burden, making the model substantially easier to train, scale for diverse patient populations, and ultimately adapt for widespread implementation in clinical environments around the world, paving the way for a more efficient and accessible form of precision cardiology.
From Lab to Clinic: Validation and Real-World Impact
Proving the Technology’s Accuracy
To rigorously validate the efficacy and reliability of their AI-driven approach, the researchers conducted a comprehensive preclinical study utilizing an established rabbit model of atherosclerosis, a condition that closely mimics human coronary artery disease. The intravascular imaging data collected via OCT was processed by the AI algorithm, and its lipid detection results were meticulously compared against histopathology, the undisputed “gold standard” in tissue analysis. This reference method involves microscopically examining thin sections of the artery that have been treated with specialized, lipid-specific stains to reveal the true biochemical composition. The comparative analysis demonstrated a remarkably high degree of accuracy, with the AI system correctly classifying image frames as either containing or lacking lipid deposits. This foundational finding confirmed the model’s core ability to reliably identify the presence of these high-risk plaques from OCT data alone.
Beyond simple binary classification, the study revealed that the AI-generated lipid maps exhibited a strong and consistent spatial correlation with the lipid deposits that were definitively confirmed through the histological examination. This critical result indicates that the model is capable of much more than just detecting the presence of lipids; it can also accurately pinpoint their precise location and map their distribution throughout the arterial wall. This spatial accuracy provides a comprehensive and clinically relevant assessment of plaque burden and vulnerability. The ability to generate such detailed biochemical maps from a non-invasive imaging technique offers an unprecedented tool for understanding disease progression and planning targeted interventions. This robust validation provides the essential evidence needed to advance the technology from the laboratory setting toward human clinical trials and eventual integration into routine cardiac care procedures.
Revolutionizing Patient Care
The prospective clinical implications of this technological advancement are profound, signaling a paradigm shift in the management of coronary artery disease towards a more predictive, preventative, and personalized standard of care. By furnishing cardiologists with real-time, objective data on plaque composition directly within the catheterization lab, this tool can substantially enhance clinical decision-making during critical procedures. For instance, a precise map of vulnerable plaques can guide the optimal length and placement of a stent, ensuring that the entire high-risk lesion is covered. This level of precision has the potential to significantly reduce the rate of post-procedural complications and lower the long-term risk of future cardiac events, ultimately leading to better patient outcomes. The technology empowers clinicians to move beyond purely anatomical assessments and incorporate crucial biochemical information into their treatment strategies.
This work stood as a powerful example of how multidisciplinary collaboration—merging expertise in optical physics, machine learning, and clinical medicine—drove the future of precision diagnostics. The innovation represented a highly accessible and cost-effective advancement because it was a software-based solution designed to work with the vast number of OCT systems already deployed in hospitals worldwide, negating the need for additional capital investment in new hardware. The research team planned to optimize the algorithm for the speed and robustness required in a fast-paced clinical setting and move toward validating its performance with human coronary artery data. Ultimately, the underlying principle of using AI to extract subtle spectral information from an imaging modality had broad applicability and could be adapted for other diagnostic tools, promising a wide-ranging impact on the fight against cardiovascular disease, one of the world’s leading causes of mortality.