In the landscape of neurodegenerative diseases, the battle is often fought against uncertainty as much as the condition itself. For those living with Motor Neurone Disease (MND), the unpredictable progression can make planning for critical interventions, like the placement of a feeding tube, an immensely stressful guessing game. Here, biopharma expert Ivan Kairatov, whose work bridges technology and clinical research, discusses a groundbreaking AI tool that promises to replace that uncertainty with data-driven foresight, fundamentally changing how clinicians and patients navigate the challenges of MND.
Timing a gastrostomy is a major challenge, with risks if it is done too early or too late. How does this AI tool help clinicians shift from reacting to MND’s progression to proactively managing it, and what does this change look like for a patient’s care journey?
This tool represents a fundamental paradigm shift in how we approach care for MND. In the past, we were often in a reactive stance, waiting for a patient’s condition to decline to a critical point—when swallowing becomes difficult and dangerous weight loss sets in. By then, the patient might be too frail, their breathing muscles too weak, making the procedure far riskier. We are now moving from crisis management to proactive, strategic planning. For a patient, this change is profound. Instead of a hurried, emergency decision made under duress, they can have a calm, thoughtful conversation with their doctor and family months in advance, feeling empowered and in control of their care plan. It’s about preserving a patient’s dignity and ensuring every decision is made to maximize their quality of life.
The model uses routine measurements from a patient’s diagnosis to predict their needs. Can you describe what types of data the AI analyzes and walk us through the step-by-step process of how it translates that information into a personalized timeline for an individual patient?
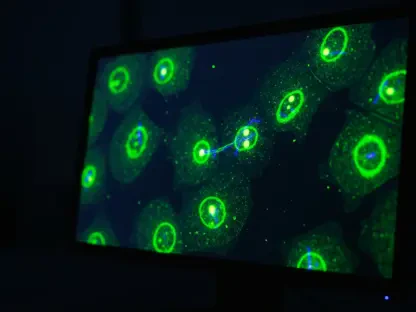
The real elegance of this model is its reliance on routine clinical measurements that are already being collected when a patient is first diagnosed. It doesn’t require invasive or specialized new tests. The AI sifts through this standard diagnostic data, drawing on patterns learned from the health journeys of over 20,000 previous patients. It identifies subtle connections and correlations that a human clinician simply couldn’t process at that scale. The system then synthesizes this information to forecast an individual’s specific disease trajectory, focusing on a key clinical indicator: the point at which significant weight loss is likely to occur. This analysis produces a personalized, predictive timeline, giving the care team a clear, actionable window for when to schedule the gastrostomy.
The tool predicts the optimal window for a feeding tube with a median error of about 3.7 months. How significant is this level of accuracy for care planning, and what happens during a patient’s six-month re-evaluation that improves the model’s precision even further?
An accuracy of within 3.7 months at the moment of diagnosis is a game-changer. Given that the timeline for needing a feeding tube can range from eight months to 20 years, narrowing it down to a three- or four-month window is an incredible leap forward. It allows for meaningful, long-term planning from day one. What’s even more impressive is how the model refines itself. When a patient comes in for their six-month re-evaluation, new data points are fed into the system. The AI then re-calibrates its prediction based on the patient’s actual progression, tightening that window of error to just 2.6 months. This iterative learning process means the forecast becomes more precise as time goes on, giving both the clinical team and the patient increasing confidence in their shared care plan.
Beyond the medical benefits, you note that uncertainty is one of the hardest aspects of living with MND. How does providing a more predictable timeline for this procedure impact the emotional and psychological well-being of patients and their families?
The psychological burden of a disease like MND cannot be overstated. Living with a constant question mark over your future is exhausting and frightening. This tool directly addresses that emotional toll by replacing the unknown with a tangible, manageable timeline. Imagine the relief for a family who can now plan their lives, arrange for support, and prepare emotionally for the next step without the constant anxiety of a potential medical crisis looming. It allows patients to focus their energy on living, rather than just worrying about what might happen next. It provides a sense of agency in a situation that can so often feel powerless, and that psychological benefit is just as vital as the physical one.
A prospective clinical trial is the next step before this tool can become standard practice. What are the key steps in a trial like this, and what specific metrics will you measure to confirm its readiness for widespread use in clinics?
A prospective clinical trial is the gold standard for validating a tool like this. The first step involves implementing the AI in a real-world clinical setting, where it will generate predictions for newly diagnosed patients. We would then track these patients over time, comparing the AI’s predicted timeline for intervention against the actual clinical need as determined by doctors. The primary metric will be accuracy: we need to confirm that the model’s predictions consistently align with patient outcomes. We’ll also measure secondary endpoints, such as patient safety, quality of life scores, and nutritional status, to ensure the proactive interventions lead to better overall health. Finally, we’ll survey both clinicians and patients to gauge their confidence in the tool and its usability in a busy clinical environment.
What is your forecast for how AI will continue to transform the management and treatment of progressive neurodegenerative diseases like MND over the next decade?
I believe we are on the cusp of a revolution. This tool is a perfect example of the immediate future: using AI for predictive, personalized care management to improve quality of life. Looking ahead, I see AI playing an even deeper role. It will accelerate drug discovery by identifying new therapeutic targets and predicting which patients are most likely to respond to specific treatments. AI will also power more sophisticated diagnostic tools, capable of detecting diseases like MND earlier and with greater accuracy. Ultimately, AI will become an indispensable partner for clinicians, processing vast amounts of data to provide insights that lead to truly personalized, proactive, and more effective treatments for these devastating diseases.