Today, we’re joined by Ivan Kairatov, a biopharma expert at the forefront of medical technology and innovation. We will be exploring the development and implications of a groundbreaking machine learning model that is reshaping our understanding of insulin resistance. Our conversation will delve into how this AI tool overcomes the limitations of traditional metrics like BMI, its startling discovery linking insulin resistance to twelve types of cancer, and what this means for the future of preventative screening and personalized medicine.
Directly measuring insulin resistance is often impractical outside of specialized clinics. Can you explain how your AI-IR model uses just nine common health checkup parameters to overcome this, and what steps were involved in validating its predictive power against direct measurements?
You’ve hit on the core challenge we aimed to solve. For years, we’ve known insulin resistance is a major health issue, but evaluating it at a population scale felt almost impossible because the direct measurement methods are so invasive and resource-intensive, really only feasible in dedicated diabetes clinics. Our AI-IR model completely changes that dynamic. We designed it to use just nine clinical parameters that are already collected during standard health checkups—things that are routine and non-specialized. By feeding these common data points into the model, we can generate a robust prediction of an individual’s insulin resistance. The validation process was incredibly rigorous; we had to prove this wasn’t just a theoretical exercise. We tested AI-IR’s predictions against validation datasets where insulin resistance had been directly measured, and the results were clear: the model achieved a strong predictive performance, giving us confidence that we had created a scalable and reliable alternative for large-scale evaluation.
Body Mass Index (BMI) is often used as a proxy for insulin resistance but can lead to false negatives. How does the AI-IR model more accurately identify at-risk individuals whom BMI might miss, and what was the process for proving its robustness to reviewers?
This is a critical point because the reliance on BMI has created significant blind spots in public health. We see “false negatives” all the time—individuals with a perfectly healthy BMI who are actually suffering from the metabolic consequences of insulin resistance. Conversely, some people with obesity are metabolically healthy. BMI is too blunt an instrument. Our AI-IR model provides a far more nuanced picture by combining those nine different clinical parameters into a single, cohesive metric. This allows it to detect the underlying insulin resistance that BMI alone simply cannot explain. Convincing our peers and reviewers of this was a major part of the research journey. We had to demonstrate, through extensive testing and data analysis, that the model was not only more powerful in its predictions but also robust under various conditions, ensuring it was a reliable tool that could overcome the well-documented shortcomings of BMI in a repeatable way.
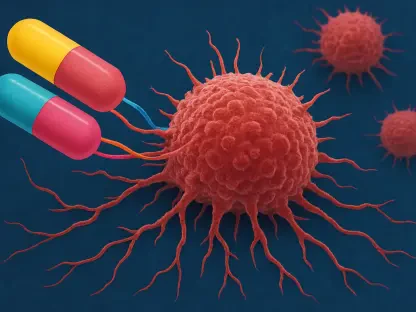
Your research identified insulin resistance as a risk factor for 12 types of cancer. Beyond establishing this link, what are the practical implications for healthcare providers, and how might this model be implemented to enable more focused screening for high-risk individuals?
Establishing that link on a population scale, using data from half a million participants, was a watershed moment. The practical implications are enormous. For healthcare providers, this moves the conversation from a vague association to a concrete, actionable risk factor. Since the nine parameters needed for the AI-IR model are obtained from standard health checkups, implementation is remarkably straightforward. A clinic could integrate this model into its existing electronic health record system. A patient’s routine bloodwork and physical exam data could automatically generate an insulin resistance score. This score would then flag high-risk individuals not just for diabetes and cardiovascular disease, but now, specifically for 12 different cancers. This allows for a much more focused and proactive screening strategy, moving us from generalized advice to targeted, personalized preventative care for those who need it most.
Now that a strong connection between insulin resistance and cancer has been demonstrated at a population scale, what are the next steps? Could you describe how you plan to investigate the influence of genetic differences and link this large-scale data to molecular biology studies?
Demonstrating the connection was the first major step, but now the real detective work begins. We want to understand the ‘why’ and the ‘how’ at a much deeper level. Our immediate next step is to explore the role of genetics. We are now working to understand how genetic differences between individuals might influence their susceptibility to developing insulin resistance and, consequently, these related cancers. The ultimate goal is to bridge the gap between this massive, population-scale human data and the intricate world of molecular biology. By linking our findings with detailed lab studies, we can begin to uncover the specific biological pathways at play. This will be crucial for developing better, more targeted strategies to overcome insulin resistance itself, rather than just managing its consequences.
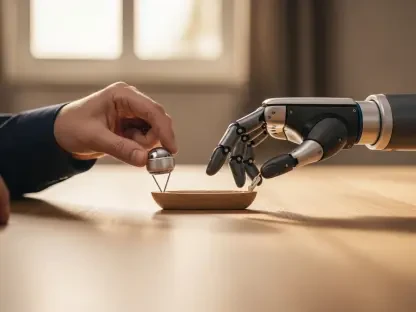
What is your forecast for the use of machine learning in preventative medicine?
I believe we are on the cusp of a complete paradigm shift, and models like AI-IR are just the beginning. My forecast is that machine learning will become the backbone of preventative medicine within the next decade. Instead of reacting to symptoms, healthcare will become predictive and proactive, identifying at-risk individuals years before a disease manifests. We will see AI integrated directly into routine checkups, analyzing complex sets of biomarkers from blood tests, genetic data, and even wearable device information to create a dynamic, holistic picture of a person’s health trajectory. This will enable truly personalized prevention plans, moving beyond generic advice to specific, data-driven recommendations that will dramatically reduce the incidence of chronic diseases like diabetes, heart disease, and many forms of cancer.