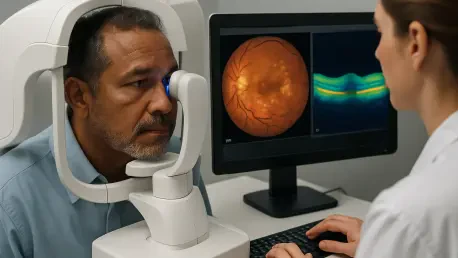
A landmark development in medical imaging is poised to transform the diagnosis of diabetic retinopathy by offering a non-invasive, AI-powered method to replace a complex and uncomfortable procedure that has long been the standard of care. This innovation addresses a critical global health issue, as diabetic retinopathy remains a leading cause of preventable blindness, and its early detection is paramount to preserving vision. Researchers have successfully created a sophisticated deep learning model, known as the UWFDR-GAN, capable of generating highly detailed angiograms of the eye’s blood vessels from a simple, non-invasive color photograph. This breakthrough eliminates the need for intravenous dye injections, making advanced retinal screening safer, faster, and significantly more accessible to millions of patients with diabetes worldwide. The technology promises to democratize a crucial diagnostic tool, potentially enabling earlier intervention and better management of this debilitating condition.
A New Frontier in Medical Imaging
The core of this technological leap lies in a powerful form of artificial intelligence called a Generative Adversarial Network, or GAN. This system was specifically engineered to perform cross-modality synthesis, which is the intricate process of creating one type of medical image from another. The model, UWFDR-GAN, was trained to learn the complex and often subtle correlations between a standard ultra-widefield color fundus photograph (UWF-CFP) and a much more detailed ultra-widefield fluorescein angiogram (UWF-FA). While the color photo shows the static structure of the retina, the angiogram reveals dynamic information about blood flow and vessel integrity. By analyzing countless pairs of these images, the AI can generate a synthetic yet diagnostically precise angiogram, complete with the critical vascular details needed for a thorough assessment, without any invasive procedures. This represents a paradigm shift from traditional imaging to AI-driven predictive visualization.
This remarkable level of realism is achieved through a unique and competitive internal process inherent to the GAN architecture. The system is composed of two distinct neural networks that work in opposition: a “generator” and a “discriminator.” The generator’s task is to create the synthetic angiogram based on the input from the color retinal photograph. Simultaneously, the discriminator, which has been trained on thousands of authentic angiograms, critically evaluates the generator’s output, trying to distinguish it from a real scan. This adversarial dynamic creates a feedback loop that constantly pushes the generator to refine its technique, improve image quality, and more accurately replicate the complex patterns of retinal vasculature. The result of this digital tug-of-war is an AI capable of producing images so faithful to reality that they preserve the minute pathological features, such as microaneurysms and vessel leakage, that are essential for an accurate diagnosis.
Proving the Potential with Validation and Accuracy
To confirm the model’s clinical viability, its creators subjected it to a rigorous validation process using an extensive dataset of paired UWF-CFP and UWF-FA images from actual patients. The performance of the UWFDR-GAN was not just based on visual inspection but was quantified using objective, industry-standard metrics, including the Structural Similarity Index (SSIM) and Peak Signal-to-Noise Ratio (PSNR). These advanced statistical tools provide an impartial measure of how closely the synthetic images match the ground-truth angiograms in terms of structural integrity, detail, and clarity. The results were exceptionally strong, indicating that the AI-generated images exhibited high fidelity and low noise, effectively bridging the gap between a non-invasive photograph and an invasive diagnostic procedure. This robust, data-driven validation is a crucial step in building the trust required for integrating such a tool into clinical practice.
The technical achievements of the model translate directly into tangible clinical benefits for both ophthalmologists and patients. The high degree of accuracy means the synthesized angiograms successfully render the subtle but critical biomarkers of diabetic retinopathy. These include the earliest signs of damage, such as tiny bulges in blood vessel walls known as microaneurysms, as well as more advanced problems like capillary non-perfusion, where small blood vessels become blocked and cease to function. The ability to visualize these features with such precision from a simple color photo is transformative. It allows clinicians to accurately stage the disease, determine its progression, and make more informed decisions about when to initiate sight-saving treatments, such as laser therapy or injections. This capability for early and precise detection is fundamental to preventing the irreversible vision loss associated with advanced stages of the condition.
Broader Impact and Future Horizons
This innovation signals a significant movement toward the democratization of advanced medical diagnostics through the power of artificial intelligence. By enabling the generation of complex angiographic data from a widely available and low-cost input like a color fundus photograph, the technology dramatically lowers the barrier to high-quality retinal assessment. In primary care settings, community clinics, or healthcare systems in resource-limited regions where specialized ophthalmological equipment and personnel are scarce, this tool could become a game-changer. It empowers a broader range of healthcare providers to conduct initial screenings for severe diabetic retinopathy, ensuring that patients who require specialist care are identified and referred far earlier than is currently possible. This enhanced accessibility is vital for implementing widespread screening programs and improving patient outcomes on a global scale.
Ultimately, the research established a powerful precedent for the future of medical AI by demonstrating a clear pathway toward more personalized and efficient healthcare. The study highlighted the remarkable adaptability of its underlying GAN architecture; while developed for diabetic retinopathy, the principles of cross-modality synthesis could readily be applied to other retinal and systemic diseases that rely on angiographic evaluation. Furthermore, the work underscored the paramount importance of clinician trust, which was addressed through rigorous validation and the production of visually coherent, clinically relevant results. This approach cemented a collaborative paradigm where AI specialists and healthcare providers worked in tandem to ensure that technological solutions were not only powerful but also patient-centric. The successful development and validation of the UWFDR-GAN served as a compelling illustration of how AI can augment clinical decision-making and redefine standards of care.