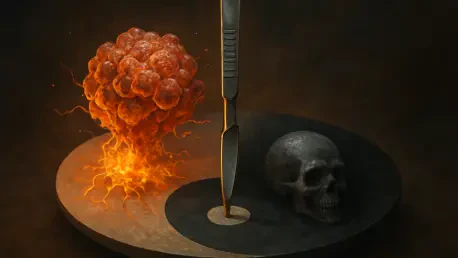
The cutting edge of cancer treatment often involves a delicate and high-stakes balance between revolutionary efficacy and severe, sometimes fatal, side effects. This reality has been starkly highlighted as a pivotal late-stage clinical trial for a promising new cancer therapy, ifinatamab deruxtecan (I-DXd), was partially halted by the U.S. Food and Drug Administration. The regulatory intervention, prompted by a troubling number of patient deaths, has cast a shadow over the drug being co-developed by pharmaceutical giants Merck & Co. and Daiichi Sankyo. This development not only raises urgent questions about the safety of this specific treatment but also puts a multi-billion dollar partnership under intense scrutiny, forcing both companies and the broader medical community to re-evaluate the risks associated with a powerful new class of targeted therapies. The outcome of the ongoing investigation will be critical in determining the future of a drug that once held immense promise for patients with a difficult-to-treat form of lung cancer.
Regulatory Scrutiny and Safety Concerns
The FDA’s Partial Clinical Hold
The U.S. Food and Drug Administration’s decision to impose a partial clinical hold on the IDeate-Lung02 trial stemmed from a deeply concerning safety signal. This large-scale Phase 3 study, which had enrolled over 500 patients diagnosed with small cell lung cancer, was designed to be the final step before a potential regulatory submission. However, an undisclosed but “higher than anticipated” number of deaths among trial participants triggered the agency’s intervention. This action brings a sudden and serious pause to a program that was advancing rapidly through the clinical development pipeline. The gravity of the situation is underscored by the fact that fatal adverse events, while a known risk in oncology trials involving critically ill patients, surpassed a predefined safety threshold, compelling regulators to step in and demand a thorough investigation into the drug’s safety profile before allowing any further patient enrollment in this critical study.
Prior to the FDA’s formal action in October, Daiichi Sankyo had already demonstrated proactive concern by initiating a voluntary pause on recruiting and enrolling new patients into the trial. The subsequent partial clinical hold formalizes this suspension, stipulating that while no new participants can join the study, patients who are already enrolled and receiving ifinatamab deruxtecan are permitted to continue their treatment. This measure is intended to protect potential new subjects from risk while allowing for the collection of further data from existing participants, which could be crucial for understanding the drug’s full safety and efficacy profile. In response, Daiichi, in close collaboration with the FDA and an independent data monitoring committee, has launched a comprehensive review of all available safety data. The primary goal of this in-depth analysis is to meticulously assess the risks, identify any potential mitigating strategies, and ultimately determine the necessary future actions for the trial and the drug’s development program as a whole.
A Known Risk Amplified
The specific cause of the patient deaths was identified as grade 5 (fatal) interstitial lung disease (ILD), a severe form of lung inflammation that can lead to scarring and irreversible damage. This adverse event is not an unknown phenomenon for Daiichi Sankyo’s technology. In fact, ILD is a recognized and significant risk associated with the company’s entire antibody-drug conjugate (ADC) platform. The company’s two commercially successful ADCs, Enhertu and Datroway, both carry prominent warnings about the potential for serious or fatal ILD on their official labeling. This history establishes a clear precedent, suggesting that the toxicity observed in the IDeate-Lung02 trial is an amplification of an inherent risk linked to the drug’s core design rather than a completely unexpected safety issue. The incident therefore underscores the persistent and formidable challenge of managing this specific side effect within this otherwise highly promising class of targeted cancer therapies, raising questions about whether the risk-benefit balance for ifinatamab deruxtecan in small cell lung cancer is acceptable.
Antibody-drug conjugates represent a sophisticated and powerful approach to cancer treatment, often described as a form of “smart chemotherapy.” These complex molecules are engineered to link a highly potent cytotoxic agent, or chemotherapy payload, directly to a monoclonal antibody. This antibody is designed to seek out and bind to specific proteins, or antigens, that are overexpressed on the surface of cancer cells. In theory, this targeted delivery mechanism allows the chemotherapy to be released directly at the tumor site, maximizing its cancer-killing effect while minimizing damage to healthy surrounding tissues. However, the case of ifinatamab deruxtecan and the associated risk of interstitial lung disease highlights the practical challenges of this technology. The precise mechanisms leading to this lung toxicity are not fully understood but serve as a stark reminder that even the most targeted therapies can have profound and sometimes deadly off-target effects, complicating their path from the laboratory to the clinic.
Broader Implications for Merck and the ADC Landscape
A Major Partnership Under Pressure
This clinical hold represents a significant setback for a therapeutic asset that is a cornerstone of a major strategic partnership between Merck and Daiichi Sankyo. In a landmark deal signed in 2023, Merck committed substantial financial resources to gain access to three of Daiichi’s leading ADC candidates, including ifinatamab deruxtecan. This agreement was a clear signal of Merck’s strategic pivot towards ADCs as a key pillar of its future oncology portfolio, aiming to build upon its success with immunotherapy and diversify its pipeline. With ifinatamab deruxtecan positioned as a near-term asset, the current safety concerns place immense pressure on the collaboration. The financial and strategic stakes are exceptionally high, and any significant delay or potential termination of this drug’s development program could have far-reaching consequences for both companies, potentially impacting investor confidence and the perceived value of the multi-drug licensing agreement.
The disappointment surrounding the trial halt is magnified by the drug’s previously stellar trajectory. Ifinatamab deruxtecan had been a source of considerable optimism, particularly after it received a coveted Breakthrough Therapy designation from the FDA. This status is reserved for drugs that have shown substantial improvement over available therapies in early clinical evidence and is intended to expedite their development and review. The designation was granted based on highly promising Phase 2 results in patients with extensive-stage small cell lung cancer, a particularly aggressive and difficult-to-treat malignancy with limited effective treatment options. The strong initial data had positioned the drug as a potential new standard of care, generating high hopes among clinicians and patients alike. This sudden pivot from celebrated front-runner to a therapy under a safety-related clinical hold creates a jarring contrast and serves as a sobering reminder of the unpredictable nature of late-stage drug development.
A Pattern of Setbacks
For Merck, this development is not an isolated incident but adds to a series of recent challenges within its ADC development program. This latest hurdle with ifinatamab deruxtecan follows a significant setback with another partnered drug, patritumab deruxtecan. In a major disappointment, Merck was forced to withdraw its approval application for that drug after a key clinical trial failed to demonstrate a clear survival benefit for patients with a specific type of non-small cell lung cancer. Compounding these clinical issues, patritumab deruxtecan had also previously faced an FDA rejection due to manufacturing concerns. This pattern of clinical and regulatory obstacles suggests that Merck is encountering significant headwinds in its ambitious effort to become a leader in the competitive ADC space. These recurring difficulties may prompt a deeper strategic review of its partnership and development strategies in this complex and high-risk therapeutic modality.
While a spokesperson for Merck confirmed that other ongoing studies of I-DXd were not directly affected by this partial hold, the immediate and long-term consequences for the pivotal IDeate-Lung02 trial became the central focus. The most pressing issue was the impact on the trial’s timeline, as the primary data readout, which had been previously anticipated in 2027, was now subject to significant uncertainty. The future of the program rested on the findings of the comprehensive safety review conducted by the companies and regulators. This investigation ultimately determined the necessary modifications to the trial protocol and the viability of continuing development. The incident served as a critical inflection point, forcing a re-evaluation of a therapy that was once seen as a major asset and highlighting the precarious journey of even the most promising drugs through the rigors of late-stage clinical validation.