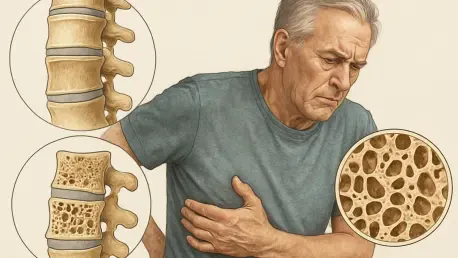
Imagine a condition so stealthy that it silently weakens bones over decades, only revealing itself through a devastating fracture that could rob a person of independence or even life—yet it’s rarely discussed in relation to half the population. Osteoporosis, long branded as a women’s health concern, poses a significant and often ignored risk to men, especially as they age. The misconception that brittle bones are a female-only issue has left countless men vulnerable to severe consequences, with many unaware of the danger until it’s too late. Shocking statistics reveal that 1 in 5 men over 50 will experience an osteoporotic fracture in their lifetime, and roughly 25% of hip fractures among older adults occur in men. This pervasive oversight in public health awareness and medical practice demands a closer look. By delving into the profound impact, screening gaps, and potential solutions, it becomes clear that addressing this hidden threat is not just necessary—it’s urgent.
Unveiling the Severity of Bone Fractures in Men
The consequences of osteoporotic fractures in men are often far graver than commonly assumed, outstripping the severity seen in women in several alarming ways. Research indicates that between 25% and 30% of men who suffer a hip fracture will die within a year, a statistic that dwarfs comparable risks in women. Beyond mortality, many survivors face permanent disability or require long-term care, stripping away independence. Perhaps most striking is the comparison to other health threats: a 50-year-old man faces a higher likelihood of death from complications of a major osteoporotic fracture than from prostate cancer. This stark reality underscores how deeply underestimated the condition remains in male populations, where the focus on other diseases often overshadows bone health. The physical and emotional toll of such injuries can reshape lives in an instant, making it imperative to shift the narrative around who is at risk.
Personal accounts add a human dimension to these sobering figures, illustrating how osteoporosis can strike unexpectedly. Consider the experience of men like Ronald Klein, who at 52 endured a broken hip and shoulder, only to discover the underlying cause was osteoporosis—a condition he never imagined could affect him. Such stories reveal a pattern of disbelief and lack of preparation among men, who often don’t suspect bone fragility until a catastrophic injury occurs. The shock of diagnosis, coupled with the grueling recovery process, highlights a critical gap in awareness. These narratives serve as a powerful reminder that the condition does not discriminate by gender, and without early recognition, men remain defenseless against its debilitating effects. Addressing this begins with acknowledging that the risk is real and pervasive, regardless of societal stereotypes.
Barriers to Detection and Diagnosis
One of the most significant hurdles in combating osteoporosis in men lies in the profound lack of awareness and inadequate screening practices. Despite the availability of diagnostic tools like the DXA scan, which measures bone density with precision, testing rates among men are dishearteningly low. Data from Veterans Affairs health centers reveals that a mere 2% of men aged 65 to 85 in a control group had undergone bone density testing, even in a system with robust resources. This gap is largely fueled by societal perceptions that frame osteoporosis as a women’s issue, leading many men to dismiss their own risk. Additionally, inconsistent clinical guidelines exacerbate the problem, with some medical bodies recommending screening for men over 70 or those with risk factors, while others cite insufficient evidence to support routine testing. The result is a patchwork approach that leaves many men unprotected.
Cultural attitudes further compound the challenge, creating a psychological barrier to diagnosis. Many men harbor a deep-seated belief in their own invulnerability, often exemplified by individuals like Bob Grossman, who resisted acknowledging the possibility of osteoporosis due to a “Superman” mentality. This mindset, rooted in traditional notions of masculinity, discourages proactive health measures and fosters denial. Compounding this is the tendency among healthcare providers to overlook the condition in male patients, focusing instead on more commonly associated risks. The interplay of personal reluctance and systemic oversight means that osteoporosis frequently goes undetected until a fracture forces recognition. Breaking through these barriers requires a dual effort: reshaping cultural narratives to normalize vulnerability and ensuring medical systems prioritize early detection for all, regardless of gender.
Promising Interventions and Steps Forward
Amid the challenges, there are glimmers of hope in the form of targeted interventions that demonstrate the power of proactive care. A notable study conducted at Veterans Affairs centers showcased the impact of establishing a dedicated bone health service, which dramatically increased screening rates to 49% among men identified as at risk. Of those tested, half were diagnosed with either osteoporosis or its precursor, osteopenia, and the majority began treatment with medications. Over an 18-month period, participants exhibited modest improvements in bone density, offering tangible evidence that structured programs can yield positive outcomes. While long-term data on fracture reduction remains under investigation, these findings suggest that systematic efforts to identify and treat at-risk individuals can shift the trajectory of bone health in men.
Expanding on this success, the potential for broader implementation of such programs holds significant promise for transforming care. Beyond screening, education plays a pivotal role in empowering men to take charge of their health. When provided with clear information about risk factors—such as family history, smoking, excessive alcohol use, or certain medications—men are more likely to engage in preventive measures. Additionally, integrating reminders into healthcare systems and ensuring provider training on male-specific risks can bridge existing gaps. The challenge lies in scaling these interventions to reach diverse populations, particularly in settings where resources or awareness are limited. Nevertheless, the evidence points to a clear path: prioritizing bone health services and fostering a culture of prevention can mitigate the devastating effects of osteoporosis before they manifest.
Systemic and Cultural Roadblocks to Overcome
Even with promising interventions, systemic and cultural obstacles continue to impede progress in addressing osteoporosis among men. Inconsistent clinical guidelines create confusion, with some experts advocating for universal screening at age 70, while others highlight a lack of large-scale trial data to justify routine testing. This discrepancy often translates to limited insurance coverage, where preventive scans like the DXA, costing between $100 and $300 out of pocket, are not reimbursed unless a fracture has already occurred. Such financial barriers deter early detection, particularly for those with limited means. Experts in the field express frustration over the glacial pace of change, noting that both policy reform and provider education lag behind the urgent need to protect aging populations from bone fragility.
Demographic shifts add another layer of complexity to this issue, as longer lifespans increase the prevalence of osteoporotic fractures. With men routinely living into their 70s and 80s, the window for bone health issues to emerge has widened significantly compared to past generations, when other causes of mortality often took precedence. This longevity, while a triumph of modern medicine, brings with it the burden of chronic conditions that complicate recovery from fractures. The intersection of aging, cumulative health challenges, and societal reluctance to address bone health in men creates a perfect storm of risk. Tackling these roadblocks demands a multifaceted approach, from revising insurance policies to ensure access to screening, to challenging ingrained cultural biases that dismiss male vulnerability.
Building a Stronger Future for Bone Health
Reflecting on the journey to recognize osteoporosis as a critical issue for men, it’s evident that past efforts laid crucial groundwork despite persistent challenges. Years of research uncovered the alarming rates of fractures and their dire consequences, with studies showing that mortality and disability struck men harder than many anticipated. Interventions tested in controlled settings, like those at Veterans Affairs centers, proved that screening and treatment could alter outcomes for the better, even if incrementally. The personal struggles of countless individuals highlighted the human cost of neglect, driving home the need for change. These milestones, though hard-won, marked a shift in understanding that bone health transcends gender.
Looking ahead, the focus must pivot to actionable strategies that build on these insights. Advocating for universal screening guidelines, especially for men over 70 or those with risk factors, could reshape preventive care. Expanding insurance coverage to include early DXA scans would remove financial hurdles, ensuring access for all. Equally vital is a cultural overhaul—public health campaigns should target men with messages that normalize seeking help for bone health. Finally, investing in research to solidify evidence on fracture prevention in men will strengthen the case for policy reform. By embracing these steps, society can safeguard aging populations, ensuring that the silent threat of osteoporosis no longer steals lives or independence from men who deserve to age with strength and dignity.