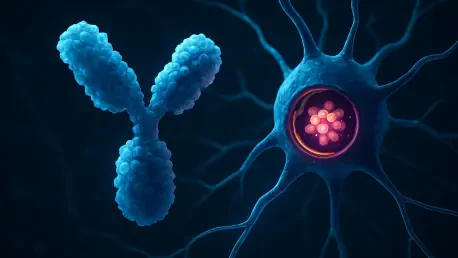
Deep within the intricate architecture of the human immune system, a component long considered a minor structural element has now been revealed as a master switch capable of fundamentally rewriting the rules of engagement for our body’s most prolific defender. For decades, the elegant Y-shaped antibody was thought to be well understood, a reliable soldier in the fight against disease. However, groundbreaking research from Japan has uncovered a previously hidden control hub within this molecule, a discovery that promises to revolutionize how therapeutic drugs are designed. This new understanding, centered on a tiny, overlooked segment, has demonstrated that a single, precise modification can transform a standard antibody into a completely new entity with finely tuned capabilities, heralding a new chapter in protein engineering.
The Architect in the Machine: A Tiny Switch Remodeling Our Body’s Best Defender
Immunoglobulin G, or IgG, stands as the most abundant antibody in the human bloodstream, comprising about 75 percent of all circulating antibodies. It is the cornerstone of the immune system’s memory, diligently recognizing and neutralizing foreign invaders like viruses and bacteria. The molecule’s classic Y-shape is a masterclass in functional design, featuring two identical “Fab” arms that specifically bind to targets and a single “Fc” stem that signals the rest of the immune system to launch an attack. This structure allows it to perform its dual role of identification and communication with remarkable efficiency.
Connecting these functional domains is the hinge region, a short, flexible segment that allows the Fab arms the freedom to move and effectively capture antigens. This hinge has a complex design, with a rigid central core flanked by pliable upper and lower segments. Historically, scientific attention has focused almost exclusively on the upper and central parts of the hinge, which contain the critical disulfide bonds that hold the antibody together. Consequently, the lower hinge was largely dismissed as a passive linker, its true importance remaining a scientific blind spot until now.
The Breakthrough: Unmasking the Lower Hinge’s True Power
A collaborative team of Japanese researchers, led by scientists at the Institute of Science Tokyo, decided to challenge this long-held assumption by systematically investigating the lower hinge’s function. Their tool of choice was trastuzumab, a widely used monoclonal antibody in cancer therapy. The team conducted a series of precise deletions, removing one amino acid at a time from this neglected region to observe the structural and functional consequences of each change.
The pivotal moment arrived with the deletion of a single proline residue at position 230 (Pro230). This minimalistic change triggered a dramatic and wholly unexpected outcome: the stable, full-sized antibody spontaneously split into two identical, stable “half-IgG1” molecules. This transformation occurred because the removal of just one amino acid was enough to disrupt the intricate pattern of disulfide bonds that normally lock the two heavy chains of the antibody together, effectively cleaving the molecule down the middle.
Redrawing the Map: A New View of Antibody Structure and Function
Advanced imaging of this novel half-antibody revealed profound structural rearrangements that went far beyond its simple division. The relative orientation between the Fab arms and the Fc stem had shifted radically. In a normal IgG molecule, the two halves of the Fc stem pair together to create a symmetrical surface that is essential for binding to immune receptors and activating a powerful response. In the half-IgG1, however, this critical signaling surface was found to be rotated inward, turning away from its potential partner and toward its own Fab region.
This inward rotation created a physical impediment, a phenomenon known as steric hindrance, where the Fab arms actively block the Fc stem from pairing correctly with another half-molecule. Despite this major structural disruption, the half-antibody was not rendered inert. It retained a partial, yet significant, ability to communicate with the immune system. The research showed that the half-IgG1 could still bind to FcγRI, a high-affinity immune receptor, through its single available interface. This monovalent interaction was sufficient to trigger a modulated immune signal, demonstrating a more nuanced level of activity compared to the all-or-nothing response of a full-length antibody.
A Blueprint for Next-Generation Medicine
This landmark study redefines the lower hinge not as a simple linker but as a decisive “structural and functional control hub” that governs the entire antibody’s architecture. The ability to generate stable half-antibodies with custom-tailored immune activity by manipulating a single amino acid presents a powerful new strategy for therapeutic design. It opens the door to creating a new class of protein-based drugs that are more specific and have fewer off-target effects.
The potential applications of this discovery are vast and promising. As Associate Professor Saeko Yanaka, a lead author of the study, explained, these findings “provide a blueprint for engineering antibody variants with tailored effector profiles for autoimmune disease, cancer, and beyond.” The principles uncovered in this research could be used to create half-antibodies that can dampen an overactive immune response in autoimmune disorders or to deliver a more focused, less aggressive signal in certain types of cancer therapy, avoiding the side effects associated with a full-blown immune activation.
The revelation of the lower hinge’s critical role had fundamentally altered the scientific understanding of antibody mechanics. This work has not only solved a long-standing mystery but also provided a tangible roadmap for developing smarter, more precise therapeutics. The capacity to fine-tune the body’s most sophisticated defenders at the molecular level marked a significant step forward, promising a future where medicines could be engineered with unprecedented control to meet the specific needs of each patient and disease.