As a leading expert in biopharma innovation, Ivan Kairatov has dedicated his career to the intersection of technology and medicine. His work focuses on pioneering new frontiers in research and development, particularly in creating intelligent therapeutic systems. Today, he shares his insights on a groundbreaking approach that leverages ultrasound and nanotechnology to turn a patient’s own tumor into a personalized vaccine factory. The conversation delves into the ingenious design of “smart” nanocatchers, the precise chemical triggers that activate them, and their profound implications for the future of cancer immunotherapy, touching upon how this strategy tackles the core challenges of tumor heterogeneity and non-specific drug delivery to create a more effective and tailored treatment.
Nanocarriers in systemic circulation often face challenges with non-specific protein binding, reducing their effectiveness. How does the S-nanocatcher’s core-shell structure address this issue, and what is the “smart switch” mechanism that activates its antigen-capturing ability precisely at the tumor site?
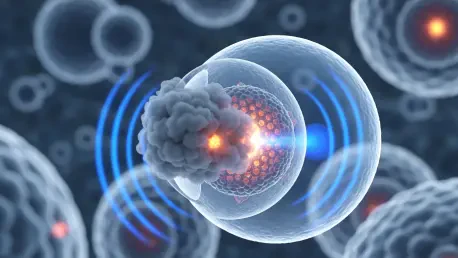
That’s the fundamental problem we have to solve in nanomedicine. When you inject a nanoparticle into the bloodstream, it’s like sending a tiny messenger into a crowded, chaotic highway. The body’s proteins immediately want to stick to it, forming a “corona” that can render it ineffective or cause it to be cleared by the immune system before it even reaches its target. The S-nanocatcher is designed for stealth. We use polyglutamic acid to create a hydrophilic, or water-loving, outer shell. Meanwhile, the critical working parts—the sonosensitizer PPA and the thioether-containing antigen-catching group, or S-ACG—are tucked away inside a hydrophobic core. This core-shell structure effectively cloaks the active components, preventing those unwanted interactions with serum proteins. It can circulate safely and invisibly until it reaches the tumor. The “smart switch” is the truly elegant part. When we focus ultrasound on the tumor, the PPA generates reactive oxygen species, or ROS. This ROS cloud oxidizes the thioether group in the core, transforming it from something that repels water to something that attracts it. This chemical flip causes the nanoparticle’s core to open up, exposing the antigen-catching group right at the moment and location it’s needed most, ensuring it only becomes “sticky” inside the tumor microenvironment.
The generation of reactive oxygen species (ROS) appears to have a dual function in this system. Could you walk us through the step-by-step process of how ROS both induces immunogenic cell death to release tumor antigens and simultaneously activates the nanocatchers to capture them?
It’s a beautifully efficient, one-two punch delivered by a single trigger. When the ultrasound is applied, the PPA within the nanocatcher core starts vibrating and producing a highly localized burst of ROS. The first job of this ROS is purely destructive, but in a very strategic way. It induces immunogenic cell death (ICD) in the surrounding cancer cells. This isn’t just quiet cell death; it’s a messy, inflammatory process that causes the tumor cells to burst open and release a flood of their internal contents, including the unique antigens that can identify them as cancerous. This creates a rich soup of personalized antigenic material right in the tumor microenvironment. At the exact same time, that very same cloud of ROS performs its second, more subtle task: it triggers the “smart switch” on the S-nanocatchers that are already present. The ROS oxidizes the thioether, activating the nanocatcher’s binding capability. So, in one swift, sonically-guided action, we are both generating the raw material for a vaccine—the antigens—and activating the tool designed to capture and process that material. It’s a synchronized event that ensures the antigens are caught immediately before they can be degraded or diffuse away.
Validating new molecular mechanisms is crucial. Could you explain how the control “C-nanocatchers,” which lacked the thioether group, helped confirm that the sulfur oxidation mechanism was essential for the system’s ability to bind antigens after being exposed to ultrasound?
In science, proving not just what happens but how it happens is paramount. The C-nanocatcher experiment was our moment of truth. To be absolutely certain that our “smart switch” was responsible for the antigen capture, we had to create a version of the nanocatcher where the switch was broken. We synthesized the C-nanocatchers to be identical to the S-nanocatchers in every way—size, structure, PPA content—with one critical exception: we replaced the sulfur-containing thioether group with a simple, inert carbon chain. This control particle could still be delivered to the tumor and, when hit with ultrasound, would still produce ROS and kill tumor cells. However, when we analyzed its performance, it showed virtually no ability to bind the released antigens. It was the “smoking gun.” This result confirmed that the capture process wasn’t some random physical adhesion caused by the ultrasound; it was entirely dependent on that specific chemical reaction—the oxidation of the sulfur group. It isolated the mechanism and gave us confidence that our design was working exactly as intended.
A 93.4% primary tumor inhibition rate is a significant outcome. What specific role did the immune adjuvant IMDQ play when combined with the S-nanocatchers, and what changes did this combination cause in the tumor microenvironment regarding dendritic cells and CD8-positive T cells?
Achieving a 93.4% inhibition rate in the primary tumor and, just as importantly, a 60% complete regression rate in distant tumors, was a remarkable validation of the system. But the S-nanocatchers couldn’t have done it alone. Think of the nanocatcher as the intelligence-gathering unit; it captures the enemy’s blueprint—the antigen. The immune adjuvant, IMDQ, is the call to arms that mobilizes the army. IMDQ is a powerful TLR7/8 agonist, which means it sends an incredibly strong “danger” signal to the immune system. When we combine it with the antigen-loaded nanocatchers, it dramatically enhances the maturation and migration of dendritic cells. These are the master coordinators of the immune response. Once activated by IMDQ and presented with the antigens from the nanocatchers, they sound the alarm. The result is a profound shift in the tumor microenvironment. It transforms from a place where the immune system is suppressed to a full-blown warzone, flooded with activated CD8-positive T cells—the “killer” T cells—and essential cytokines like IFN-γ and TNF-α. This orchestrated attack is what leads to such potent tumor destruction, both locally and systemically.
Tumor heterogeneity complicates the development of universal cancer vaccines. How does this in-situ capture strategy, which uses a patient’s own unique antigens, provide a more personalized and precise platform compared to traditional vaccine approaches that require external antigen identification and synthesis?
This gets to the very heart of why this technology is so exciting. The immense diversity of tumors, not just between patients but within a single patient, is one of the biggest hurdles in oncology. Traditional vaccine development is a laborious process. You have to biopsy a tumor, take it to a lab, spend weeks or months trying to identify which antigens might provoke an immune response, and then manufacture a vaccine based on that limited snapshot. By the time it’s ready, the tumor may have already evolved. Our in-situ strategy sidesteps that entire logistical and scientific bottleneck. We don’t need to know the identity of the antigens in advance. We send the nanocatchers directly to the source. They capture the full, complex spectrum of antigens being released by that patient’s tumor, in real-time. This creates a completely bespoke vaccine that is perfectly matched to the individual’s specific cancer at that specific moment. It’s a paradigm shift from a one-size-fits-all approach to a truly personalized, dynamic, and precise form of immunotherapy.
What is your forecast for the future of in-situ vaccine development using stimuli-responsive nanomaterials?
I am exceptionally bullish on this approach. I believe we are witnessing the dawn of a new class of “smart” therapeutics that can actively sense and respond to their environment. The future isn’t just about single-stimulus systems like this one; I foresee the development of multi-responsive platforms. Imagine a nanoparticle that is triggered not only by ultrasound but also by the unique pH or enzyme profile of a tumor, adding layers of specificity and control. We’ll also see these in-situ vaccine platforms combined with other powerful immunotherapies, such as checkpoint inhibitors, to create synergistic effects that can overcome even the most stubborn treatment resistance. The ultimate vision is a system where we can non-invasively treat a primary tumor and, in doing so, generate a potent, systemic immune response that hunts down and eliminates metastatic disease throughout the body. This technology provides a tangible pathway to making personalized cancer vaccines a widespread clinical reality, transforming how we fight this incredibly complex disease.