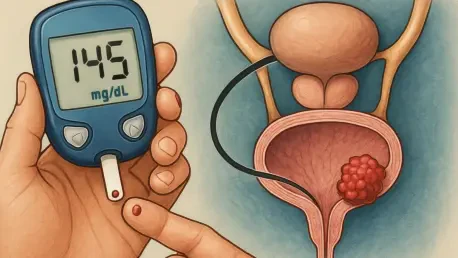
The alarming statistic that individuals with type 1 diabetes face a 4.29-fold increased risk of developing bladder cancer has sent ripples through the medical community, challenging long-held assumptions about the intersection of metabolic disorders and malignancies. With bladder cancer already impacting roughly 2% of the U.S. population, understanding how a chronic condition like type 1 diabetes amplifies this risk is critical. This roundup gathers diverse perspectives from researchers, clinicians, and health advocates to explore the implications of this link, compare varying viewpoints on its causes, and provide practical advice for those affected. The goal is to distill complex insights into actionable information for patients and providers alike.
Uncovering the Link: Diverse Research Perspectives
Recent studies have brought to light a significant association between type 1 diabetes and an elevated risk of bladder cancer, prompting varied interpretations among researchers. Many epidemiologists emphasize the methodological breakthrough of adjusting for confounding factors like smoking, which obscured this connection in earlier analyses. By integrating comprehensive data sets and refining statistical models, these studies have isolated type 1 diabetes as an independent risk factor, sparking discussions about why this link remained hidden for so long.
On the other hand, some researchers caution that while the statistical association is clear, the biological mechanisms driving this risk are still under investigation. Theories range from chronic inflammation associated with diabetes to potential effects of long-term insulin therapy, but consensus remains elusive. This uncertainty has led to calls for interdisciplinary collaboration, with experts advocating for studies that merge oncology and endocrinology to pinpoint how metabolic disruptions might fuel cancer development.
A third viewpoint focuses on the historical oversight in research design, particularly the failure to account for behavioral differences among diabetes patients. Some scholars argue that healthier lifestyle choices, such as reduced smoking rates among those diagnosed early with type 1 diabetes, masked the true risk in past datasets. This perspective highlights the need for future research to incorporate nuanced behavioral data, ensuring more accurate risk assessments.
Clinical Voices: Implications for Patient Care
Healthcare providers offer a spectrum of opinions on how this elevated bladder cancer risk should reshape care for type 1 diabetes patients. A common theme among clinicians is the urgent need for heightened awareness of early cancer symptoms, such as blood in the urine or frequent urinary issues. Many suggest that routine screenings or discussions about bladder health should become standard during diabetes check-ups, especially for patients with additional risk factors like a history of smoking.
Diverging slightly, some medical professionals stress the importance of preventive strategies over reactive measures. They advocate for aggressive smoking cessation programs tailored specifically for diabetes patients, noting that the combined effect of smoking and diabetes may exponentially increase cancer risk. Educational campaigns to reinforce the dangers of tobacco use, even in small amounts, are seen as a vital tool in reducing this compounded threat.
Another clinical perspective centers on the integration of cancer prevention into broader diabetes management plans. Providers in this camp argue for a holistic approach, where tight blood sugar control and regular health monitoring are paired with discussions about cancer risk. This view pushes for updated clinical guidelines that address both metabolic and oncological concerns, ensuring patients receive comprehensive care that tackles multiple health fronts.
Health Advocates Weigh In: Practical Tips for Risk Reduction
Health advocates and patient support groups provide a grassroots perspective, focusing on actionable steps for individuals with type 1 diabetes to mitigate their bladder cancer risk. One widely shared tip is the prioritization of smoking cessation, with many organizations offering resources like counseling or support groups to help patients quit. They emphasize that even reducing exposure to secondhand smoke can make a tangible difference in lowering risk.
Another key piece of advice revolves around maintaining strict control over blood sugar levels, as fluctuations may contribute to systemic inflammation—a potential factor in cancer development. Advocates encourage patients to work closely with healthcare teams to fine-tune insulin regimens and adopt diets that stabilize glucose levels. This proactive stance empowers individuals to take charge of their health beyond just diabetes management.
A less commonly discussed but equally important suggestion is fostering open dialogue with healthcare providers about personal risk profiles. Advocacy groups urge patients to ask pointed questions during medical visits, such as whether specific symptoms warrant further investigation or if preventive screenings are advisable. This approach aims to bridge the gap between research findings and personal health strategies, ensuring that individuals feel informed and supported.
Navigating the Future: What Lies Ahead
Reflecting on this roundup, it becomes evident that the connection between type 1 diabetes and bladder cancer has stirred a wide array of reactions from researchers, clinicians, and advocates. The consensus on a 4.29-fold increased risk underscores a shared urgency to address this issue, though opinions differ on the root causes and immediate responses. While researchers debate biological pathways, clinicians push for enhanced vigilance, and advocates provide hands-on tips for risk reduction.
Looking ahead, a promising next step involves diving deeper into educational resources and support networks focused on chronic conditions and cancer prevention. Exploring studies or programs that bridge metabolic health and oncology could offer fresh perspectives for those affected. Encouraging ongoing conversations with healthcare providers about tailored prevention plans emerges as a critical action, ensuring that this newfound risk does not remain an abstract statistic but transforms into meaningful change in patient care.