When a lifesaving transplant risks unleashing the very immune fire meant to cure leukemia, choices about how to steer immunity before donor cells arrive determine whether patients heal or face harm. That dilemma sits at the heart of allogeneic hematopoietic stem cell transplantation, where graft-versus-host disease (GVHD) must be prevented without dimming the graft-versus-leukemia (GVL) effect that keeps cancer at bay.
Recent preclinical work set up a head-to-head conceptual comparison: priming recipient regulatory T cells (Tregs) in vivo using TL1A-Ig plus low-dose interleukin-2 versus relying on conventional broad immunosuppression. The former wagers on precision and tissue preparation; the latter leans on time-tested systemic dampening. What follows assesses how these approaches align with modern transplant priorities and where they diverge.
Foundations, context, and relevance
The two strategies share a single goal—prevent GVHD—yet they differ in philosophy. Treg priming uses dual-receptor targeting of TNFRSF25 and CD25 to expand and activate recipient Tregs before transplant, aiming to build tolerance where damage usually starts. Broad immunosuppression, in contrast, employs calcineurin inhibitors, methotrexate, mycophenolate, corticosteroids, or post-transplant cyclophosphamide to blunt donor T cell activation after graft infusion.
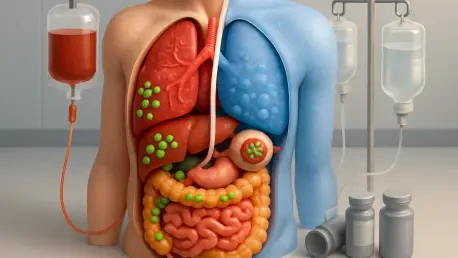
This contrast matters because GVHD remains the chief barrier to safer transplantation, and every intervention must protect GVL. Treg priming proposes conditioning host tissues—colon, liver, and eye included—so donor cells meet a regulated landscape. Standard prophylaxis counters activation systemically, which controls GVHD but often taxes pathogen defense, vaccine responses, and sometimes anti-leukemia activity.
Scope and maturity also differ. Treg priming currently rests on preclinical evidence showing Treg expansion, tissue homing, and preserved GVL, alongside signals of a healthier gut microbiome. Broad immunosuppression anchors today’s care, guided by established dosing schemas, drug levels, and clinician experience. The practical question is not whether to abandon standard prophylaxis, but how a mechanism-based, pretransplant add-on could rebalance efficacy and safety.
Comparative evaluation across core dimensions
Mechanism and selectivity of immune modulation
Treg priming takes aim at specificity. TL1A-Ig co-stimulation through TNFRSF25 synergizes with low-dose IL-2 signaling via CD25 to preferentially grow and activate Tregs in vivo. Crucially, this priming occurs before donor cells arrive, allowing Tregs to accumulate in GVHD-prone tissues and shape local immunity without globally silencing effector functions.
Broad immunosuppression operates through systemic pressure. Calcineurin blockade and antimetabolites reduce T cell activation and proliferation across lineages, while steroids suppress inflammation broadly. These levers reliably reduce early alloreactivity, yet they do so with little regard for tissue context, and they frequently suppress beneficial anti-tumor and antimicrobial responses.
Selectivity thus becomes the dividing line. Treg priming seeks to modulate harmful alloreactivity and spare GVL, whereas broad immunosuppression trades precision for certainty, accepting collateral dampening of multiple immune circuits. The result is a comparison between surgical restraint and blanket control.
Efficacy, safety, and biological outcomes
Preclinically, Treg priming produced a favorable constellation of outcomes: improved survival, lower clinical GVHD scores, less weight loss, and preserved histology in vulnerable organs. Notably, anti-leukemia activity persisted, indicating that the approach throttled alloaggression without muting cytotoxic immunity. A parallel observation—greater gut microbial diversity—aligned with a more resilient immune ecosystem.
Standard prophylaxis, by contrast, has a long record of reducing GVHD across risk groups, especially when regimens are optimized for timing and combination. Yet the price often includes infections, viral reactivation, organ toxicities, and metabolic side effects. In some settings, GVL is attenuated, nudging relapse risk upward and prompting cautious tapering that can invite late GVHD.
Microbiome impacts reveal another split. Broad immunosuppression, compounded by antibiotic exposure, frequently narrows microbial diversity, which correlates with worse GVHD. Treg priming’s association with a richer microbiome suggests a bidirectional benefit: better barrier integrity and gentler inflammatory tone that together stabilize early immune recovery.
Practicality, scalability, and implementation pathways
In vivo Treg priming avoids ex vivo collection or engineering, pointing to scalability and standardization if safety and dosing translate clinically. A defined, time-bound pretransplant protocol could slot into existing workflows and be tracked with biomarkers such as circulating Treg frequencies, tissue-homing signatures, and microbiome metrics.
Broad immunosuppression, meanwhile, is straightforward to deliver and widely reimbursed. Clinicians already manage drug levels, interactions, and dose adjustments, making implementation predictable. However, the cumulative burden—organ toxicity, infection surveillance, and prolonged tapering—adds complexity and resource load over time.
The implementation calculus therefore depends on institutional capacity. Programs equipped for immune monitoring and microbiome stewardship could trial a priming-first approach with minimized baseline suppression, while centers favoring standardized playbooks may continue to optimize established regimens and taper strategies.
Challenges, limitations, and key considerations
Treg priming faces the usual translational hurdles. Human safety, dose, and the durability of benefit remain unproven, and selectivity could fade if IL-2 exposure expands non-Treg populations. Patient heterogeneity, conditioning intensity, and concurrent prophylaxis may sway outcomes, while manufacturing TL1A-Ig and deploying companion diagnostics will require clear standards.
Conventional suppression carries its own liabilities. Infection risk, impaired vaccine responses, organ toxicities, and cytopenias are expected trade-offs, and relapse concerns persist where GVL is blunted. Tissue repair can lag under systemic steroids and antimetabolites, potentially undermining barrier function precisely when microbial homeostasis matters most.
Operational variability further complicates comparisons. Regimen choices differ across centers, and cumulative exposure to multiple agents makes attribution difficult. These realities underscore why a mechanism-based, pretransplant strategy draws interest: it promises front-loaded precision that might reduce downstream complexity.
Synthesis, recommendations, and decision guidance
The balance of evidence sketched a clear narrative. Treg priming offered targeted, tissue-aware regulation with preserved GVL, improved organ integrity, and favorable microbiome signals in preclinical models. Broad immunosuppression remained effective and accessible but continued to exact costs in infections, toxicities, and, at times, relapse risk.
Practical recommendations followed. In settings where GVL preservation was paramount or infection risk was high, Treg priming deserved evaluation as an adjunct or as a platform for reducing systemic exposure. Hybrid designs—priming plus minimized baseline prophylaxis—were well aligned with adaptive tapering guided by Treg and microbiome biomarkers.
Candidate profiles included patients with prior intolerance to immunosuppressants, comorbidity-driven infection vulnerability, or malignancies where cytotoxic control could not be compromised. Programs considering this path needed capacity for immune monitoring, microbiome stewardship, and disciplined pretransplant scheduling to capture the timing advantage.
Next steps were concrete. Early-phase trials were prioritized to define dose, timing, and patient selection, with endpoints spanning GVHD, infections, relapse, survival, and microbiome indices. Correlative studies on tissue Treg homing and durability, plus health-economic analyses, would have clarified scalability and value relative to standard prophylaxis. As the field moved toward mechanism-based prevention, this comparison pointed toward a future in which GVHD control and GVL retention coexisted more reliably.