In the heart of Sudan, a nation gripped by unrelenting conflict, the provision of medical care, particularly anesthesia for surgical procedures, teeters on the edge of collapse due to systemic challenges and ongoing violence that have devastated infrastructure and resources. The city of Wad Medani in Gezira State has emerged as a critical case study for understanding how healthcare systems struggle to operate under the immense strain of war, where hospitals are destroyed and supplies are scarce. Here, non-physician anesthesia providers (NPAPs), often with limited formal training, have been thrust into roles typically reserved for specialized physicians, filling a gaping void left by a severe shortage of anesthesiologists. With conflict displacing medical experts and demolishing key hospitals, these providers frequently stand as the sole barrier between life and death for patients requiring urgent surgical intervention. This article delves into the precarious realities and inherent risks of task-sharing anesthesia in such extreme conditions, drawing on a pivotal study conducted between 2022 and 2023 across four major referral hospitals in Wad Medani. By analyzing over 1,500 surgical cases, the research exposes stark safety gaps and systemic breakdowns that jeopardize lives daily. These findings serve as a critical alert, not only for Sudan but for any conflict zone grappling with the monumental task of sustaining healthcare amidst chaos and destruction.
A Healthcare System Under Siege
Sudan’s healthcare framework was already fragile before the escalation of conflict in 2023, with a mere 0.47 anesthesiologists per 100,000 people—a figure that falls dramatically short of global benchmarks for safe surgical care. This scarcity, already a significant barrier in peacetime, has been compounded by the war, which has displaced between 70% and 80% of the country’s trained anesthesiologists, many of whom were forced to flee as hospitals in Khartoum were reduced to rubble. The resulting vacuum has left regions like Wad Medani in a desperate state, where the demand for surgical services continues to rise amid an influx of war-wounded patients. The burden of care has shifted almost entirely to NPAPs, including technologists and technicians, who now constitute 93% of the anesthesia workforce across the hospitals studied. This overwhelming reliance on non-physician providers is a stark indicator of a system pushed beyond its limits, struggling to maintain even basic levels of medical service in the face of unrelenting adversity.
The depth of this crisis is evident in the stark disparities within healthcare facilities, where some hospitals, such as the National Centre for Paediatric Surgery in Wad Medani, operate without a single physician anesthesiologist on staff. Among a workforce of 99 providers across four major referral centers, only seven are trained specialists, leaving NPAPs to manage nearly half of all surgical cases independently. This dependency is not a choice but a necessity, born from the harsh realities of conflict that have stripped away resources and expertise. These providers have become the linchpin of surgical care, often working in high-pressure environments with minimal support, handling emergency procedures and routine surgeries alike. The situation underscores a broader challenge faced by many low- and middle-income countries, amplified in Sudan by the destructive force of war, where the absence of specialists threatens the very foundation of medical care delivery.
Balancing Necessity and Danger in Task Delegation
Task-sharing and task-shifting have emerged as critical, yet problematic, strategies to address the acute shortage of anesthesia specialists in Sudan’s conflict zones. Task-sharing involves NPAPs working alongside physicians in a collaborative setting, while task-shifting sees them taking on full responsibility for cases without direct supervision, a practice endorsed by global health bodies as a stopgap measure in resource-poor areas. In Wad Medani, these approaches are often implemented informally, with NPAPs independently managing 46% of surgical cases due to the sheer unavailability of specialists. They handle critical procedures, performing 82% of intubations and 91% of spinal anesthetics, demonstrating their indispensable role in maintaining the flow of surgical services under dire circumstances. However, the lack of structured guidelines or formal oversight introduces significant inconsistencies in care delivery, creating a precarious balance between necessity and risk.
This informal division of labor often reserves physician involvement for complex cases, while NPAPs are tasked with routine procedures, such as spinal anesthesia for cesarean sections, in an effort to maximize limited resources. While the intent behind this stratification is to optimize efficiency in a strained system, it can lead to severe consequences when seemingly straightforward cases take unexpected turns without immediate access to expert intervention. The absence of a regulated framework defining the scope of practice for NPAPs means that many operate in a gray area, lacking the legal or institutional backing needed to ensure consistent quality of care. In a conflict setting, where every procedure carries heightened risk due to disrupted infrastructure, this ad-hoc approach to task delegation often transforms a pragmatic solution into a dangerous gamble, highlighting the urgent need for formalized protocols to safeguard patient outcomes.
Unsupervised Care and Escalating Patient Risks
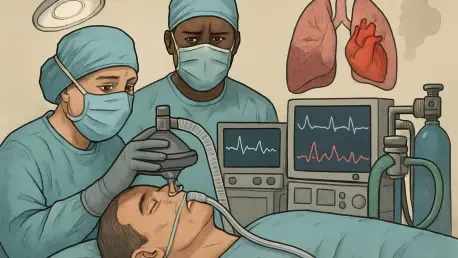
One of the most alarming revelations from the Wad Medani study is the significant disparity in patient safety outcomes between supervised and unsupervised anesthesia care provided by NPAPs. Adverse events occur in 34% of cases managed independently by these providers, a rate nearly three times higher than the 12% seen when a physician is present to oversee the procedure. This striking risk ratio underscores the critical importance of supervision in mitigating complications, particularly in a high-stakes environment where errors can be fatal. The most prevalent issues in unsupervised settings include cardiovascular instability, often linked to spinal anesthesia and accounting for 58% of adverse events, a condition that can rapidly escalate without prompt intervention. These statistics paint a grim picture of the challenges faced by NPAPs working alone under immense pressure.
Further compounding the danger are other frequent complications such as airway and respiratory crises, alongside significant hemorrhage, which also spike dramatically in the absence of oversight. These risks are not a reflection of individual shortcomings among NPAPs but rather a symptom of broader systemic failures, including the lack of immediate access to senior support and critical resources like emergency medications. In a conflict zone, even routine procedures become hazardous when supply chains for essential drugs are disrupted and specialists are displaced or unavailable. The heightened surgical demand from war-related injuries adds another layer of complexity, stretching already thin resources to the breaking point. This situation reveals a harsh truth: without robust support structures, the reliance on unsupervised NPAPs, while necessary, places patients at an unacceptably high risk of preventable harm.
Systemic Breakdowns Amplifying the Crisis
Beyond the immediate risks of unsupervised care, the study uncovers profound systemic failures that undermine the safety and efficacy of anesthesia services in Sudan’s conflict-affected regions. A staggering 94% of adverse events go undocumented in patient records, rendering the majority of complications invisible to the formal healthcare system and preventing any meaningful opportunity for learning or improvement. This near-total breakdown in reporting is compounded by the fact that only a small fraction of incidents are escalated to senior providers for review or intervention, effectively severing the clinical safety loop essential for quality care. Such gaps in documentation are not mere administrative oversights but a critical barrier to addressing recurring issues, perpetuating a cycle of hidden risks that endanger lives on a daily basis.
Equally troubling is the complete lack of access to continuing education for NPAPs, leaving them ill-equipped to adapt to evolving medical challenges or refine their skills over time. This educational void exists alongside other systemic shortcomings, including chronic shortages of equipment and medications, as well as the absence of regulatory frameworks to guide and protect non-physician providers. The ongoing conflict has exacerbated these issues to a catastrophic level, with infrastructure destruction, personnel displacement, and severed supply lines creating an environment where even the most basic standards of care are unattainable. These systemic breakdowns are not unique to Sudan but are magnified in a war-torn context, where the simultaneous collapse of multiple support systems transforms manageable challenges into life-threatening crises for both patients and providers.
Pathways to Reform in Conflict Settings
Addressing the dire state of anesthesia care in Sudan’s conflict zones requires urgent, tailored interventions that acknowledge the unique constraints of a war-torn environment. The Wad Medani study calls for formalizing the roles of NPAPs through clear legislation, drawing inspiration from successful models in other low- and middle-income countries where defined scopes of practice have improved accountability and safety. Such legal frameworks would provide clarity on responsibilities and offer protection to non-physician providers, reducing the ambiguity that currently heightens risks. Additionally, integrating NPAPs into national surgical plans and humanitarian response strategies is essential to ensure their contributions are recognized and adequately resourced, even amidst ongoing conflict. These structural reforms are vital first steps toward building a more resilient healthcare workforce capable of withstanding crisis conditions.
Innovative solutions leveraging technology also hold significant promise for bridging critical gaps in supervision and support. The use of mobile platforms for remote consultation, such as real-time guidance via messaging apps, could connect NPAPs with distant specialists, offering a lifeline in areas where physical oversight is impossible. Investment in training programs, even if delivered through virtual or mobile formats, is another actionable measure to enhance skills and confidence among non-physician providers. These interventions must be backed by dedicated humanitarian funding, as standard health budgets in conflict zones are often insufficient to tackle the scale of systemic failures. By combining legislative clarity with technology-driven support and professional development, there is potential to transform the current landscape of anesthesia care in Sudan, turning a patchwork of desperate measures into a sustainable system that prioritizes patient safety despite the surrounding chaos.
Reflecting on Lessons for Global Health
Looking back, the challenges faced by NPAPs in Sudan’s conflict zones during the 2022-2023 study period offered a sobering glimpse into the fragility of healthcare systems under siege. The stark contrast in adverse event rates between supervised and unsupervised care highlighted a fundamental truth: necessity alone cannot justify the risks borne by patients when systemic support is absent. The near-total failure to document complications and the absence of educational opportunities for providers painted a picture of a system not just strained, but broken by the compounded effects of war. These findings echoed broader struggles in fragile states worldwide, where conflict acts as a multiplier of pre-existing health disparities, turning manageable shortages into deadly crises.
Moving forward, the path to safer anesthesia care in such environments lies in immediate, context-specific actions that build on global best practices while adapting to local realities. Prioritizing the development of mobile supervision tools can provide a rapid response to the isolation faced by NPAPs, ensuring they are not left to navigate complex cases alone. Simultaneously, advocacy for international support to fund training initiatives and rebuild infrastructure must gain momentum, recognizing that long-term stability depends on equipping local providers with the tools to succeed. These steps, paired with a commitment to integrating lessons from Sudan into global health frameworks, can pave the way for more resilient surgical systems in conflict zones, ensuring that even in the darkest of times, the right to safe medical care remains within reach for all.