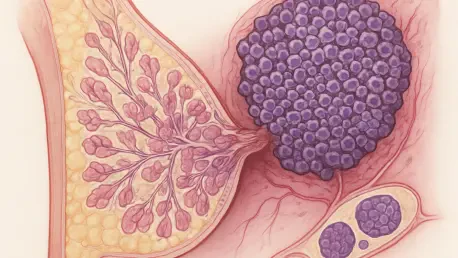
Triple-negative breast cancer (TNBC) remains one of the most formidable challenges in oncology, characterized by its aggressive nature and lack of the three common receptors—estrogen, progesterone, and HER2—that many standard therapies target, leaving patients with limited treatment options and often dismal survival rates. This absence of receptors, combined with TNBC’s high propensity to metastasize and spread to distant organs like the lungs or brain, makes it a particularly deadly form of cancer. A groundbreaking study from Weill Cornell Medicine has recently shed light on a potential game-changer in this fight, identifying the enzyme EZ## as a critical driver of TNBC’s deadly spread. By focusing on inhibiting this epigenetic regulator, researchers propose a novel strategy to restore normal cell division and prevent metastasis, offering a glimmer of hope for those affected by this devastating disease. The findings challenge traditional cancer treatment paradigms and suggest that a more balanced approach could yield better outcomes for patients facing such a relentless adversary.
Unraveling the Role of EZ## in Cancer Progression
The research from Weill Cornell Medicine zeroes in on EZ##, an enzyme that plays a pivotal role in epigenetic regulation, altering how genes are expressed without changing the DNA sequence itself. In TNBC, EZ## is overproduced, particularly in a small but highly dangerous subset of tumor cells—roughly 5% of the primary tumor—that are primed to metastasize. These cells exhibit unique characteristics, such as altered metabolism and significant chromosomal instability, which refers to errors during cell division that result in uneven chromosome distribution. This genetic disarray fuels the cancer’s ability to spread to other parts of the body. By silencing genes essential for proper chromosome segregation, EZ## disrupts the delicate balance of cell division, creating an environment where cancer cells thrive and invade distant sites. The study’s focus on this specific enzyme marks a departure from broader, less targeted approaches, highlighting a precise mechanism behind TNBC’s aggressive behavior.
Delving deeper into the mechanics, EZ##’s impact on chromosomal instability becomes clearer through its interaction with specific genetic pathways. The enzyme silences the tankyrase 1 gene, which normally supports the machinery responsible for evenly splitting chromosomes into daughter cells during division. Without this regulation, a protein known as CPAP accumulates, leading to an overabundance of centrosomes—structures critical for organizing cell division. This results in abnormal splits, where cells divide into three or more offspring instead of the usual two, amplifying genetic errors that enhance metastatic potential. The research demonstrates that targeting EZ## could interrupt this destructive cycle, potentially halting the spread of TNBC at its source. This mechanistic insight provides a compelling rationale for developing therapies aimed at this enzyme, as it addresses a root cause of the cancer’s lethality rather than merely its symptoms.
Pioneering a New Treatment Strategy
A significant trend in modern cancer research is the shift toward targeting epigenetic factors like EZ## to address the underlying drivers of disease progression, rather than solely focusing on destroying tumor cells. The Weill Cornell study aligns with this movement, showing promising preclinical results with EZ## inhibitors, including the FDA-approved drug tazemetostat. In TNBC cell lines and mouse models, these inhibitors have successfully reduced chromosomal instability and curbed metastasis, suggesting a viable path forward for human application. Analysis of patient data further supports this approach, revealing a strong correlation between elevated EZ## levels and increased chromosomal alterations in tumor samples. Such findings validate EZ## as a critical therapeutic target and underscore the potential of repurposing existing drugs to tackle one of the most challenging forms of breast cancer, offering a faster route to clinical impact.
Beyond the laboratory, the emphasis on preventing metastasis before it occurs resonates strongly with clinical needs, as this remains the primary reason for poor survival rates among TNBC patients. The research team advocates for a paradigm shift in treatment strategies, moving away from methods that risk exacerbating tumor aggressiveness through induced instability. Instead, restoring cellular balance via EZ## inhibition presents a safer, more controlled alternative. Insights from surgical oncologists involved in the study highlight the devastating toll of metastasis on patients, reinforcing the urgency of translating these findings into real-world therapies. With drugs like tazemetostat already approved for other cancers, there is cautious optimism that refining or repurposing these agents could soon provide a much-needed lifeline for those battling TNBC, potentially transforming survival outcomes in the near future.
Future Directions in TNBC Therapy
The implications of targeting EZ## extend far beyond the immediate findings, opening doors to innovative therapeutic avenues for TNBC and possibly other cancers with similar characteristics, such as lung adenocarcinoma. The study suggests that clinical trials testing EZ## inhibitors in high-risk breast cancer patients should be a priority, given the preclinical success and the existing availability of drugs like tazemetostat. Such trials could pave the way for personalized treatment plans, identifying patients with elevated EZ## levels who might benefit most from this approach. Additionally, the research underscores the broader potential of epigenetic therapies in cancer management, shifting the focus from merely treating primary tumors to proactively preventing their deadly spread. This represents a significant evolution in how aggressive cancers are approached, prioritizing long-term control over short-term destruction.
Looking ahead, the challenge lies in optimizing EZ## inhibitors to maximize efficacy while minimizing side effects, ensuring they can be safely integrated into clinical practice. Collaborative efforts between researchers, clinicians, and pharmaceutical developers will be crucial in refining these therapies and accelerating their journey from bench to bedside. The study also calls for further exploration into other epigenetic regulators that might play complementary roles in TNBC progression, potentially leading to combination therapies that enhance outcomes. As the fight against TNBC continues, the focus on EZ## offers a beacon of hope, suggesting that a deeper understanding of cellular mechanisms can unlock new strategies to combat metastasis. This research marks a pivotal step forward, setting the stage for a future where even the most aggressive cancers might be managed with precision and care.