The aftermath of a spinal cord injury unleashes a devastating and prolonged biological assault, where the secondary damage cascade often proves more destructive than the initial physical trauma. This secondary injury process is a complex storm of excessive reactive oxygen species, relentless inflammation, and widespread programmed cell death, which together create a hostile microenvironment that actively thwarts any attempts at neural regeneration. Despite the best efforts of modern medicine, including surgery and intensive rehabilitation, long-term functional recovery remains severely limited for a majority of patients. Many experimental therapies have historically fallen short, largely because they adopt a narrow, single-target approach that is fundamentally ill-equipped to combat the multifaceted nature of the injury. This persistent challenge has solidified a consensus within the scientific community: meaningful progress will necessitate multi-target regulatory strategies that can simultaneously address the key pathological drivers of this debilitating condition.
A Landmark Study in Synergistic Therapy
The Luteolin-Astragaloside IV Combination
In a groundbreaking study published late in 2025 in the journal Precision Clinical Medicine, a collaborative research team has illuminated a promising new path forward by harnessing the power of a synergistic drug-pair therapy. The investigation focused on the combined therapeutic potential of luteolin and astragaloside IV, two bioactive compounds with well-established roots in traditional herbal medicine. The primary objective of the research was to meticulously determine if this dual-compound strategy could significantly outperform single-compound treatments in fostering neural repair and restoring motor function following a severe spinal cord injury. By implementing a rigorous two-stage methodology that encompassed both cellular and animal models, the scientists have presented compelling evidence that the luteolin-astragaloside IV combination effectively enhances recovery by concurrently mitigating oxidative stress and neuroinflammation, thereby reshaping the post-injury landscape into one that is far more conducive to healing and regeneration.
Validation at the Cellular Level
The initial phase of the investigation was conducted using an in vitro cellular model meticulously designed to simulate the intense oxidative stress that neurons endure in the wake of an injury. In this controlled laboratory setting, the researchers observed that when applied individually, neither luteolin nor astragaloside IV offered any substantial neuroprotective benefits. The neuronal cells, when exposed to oxidative conditions, showed little improvement in survival with either single compound. However, a powerful synergistic effect emerged when the two compounds were administered in combination. This dual-drug therapy resulted in a significant reduction in the accumulation of harmful reactive oxygen species and led to a marked improvement in the overall survival rates of the stressed neuronal cells. This crucial initial finding provided a clear and robust validation of the drug pair’s synergistic antioxidant potential, establishing a strong scientific foundation to justify advancing the study into more complex, in-vivo animal models.
The success of the combination therapy at the cellular level pointed toward a complementary mechanism of action, where each compound addresses a different facet of the oxidative stress pathway, creating a more comprehensive defense than either could alone. This synergy is critical because the oxidative burst following SCI is not a simple, monolithic event but a complex cascade involving multiple enzymatic and non-enzymatic sources of reactive oxygen species. By targeting this network from multiple angles, the luteolin-astragaloside IV pair effectively dismantled the destructive cycle at its core. This ability to neutralize a broad spectrum of oxidative threats is what likely underpins its superior performance compared to single-agent approaches. The data from these cellular experiments were not just a preliminary step but a vital proof-of-concept, demonstrating that a multi-target strategy was indeed a viable and potent method for protecting vulnerable neural tissue in a simulated post-injury environment, paving the way for subsequent animal trials.
From Cellular Success to Functional Recovery
Remarkable Improvements in Animal Models
Building upon the highly encouraging results from the cellular trials, the research team transitioned their investigation to a clinically relevant rat model of severe spinal cord contusion injury. In this pivotal phase, a single, localized injection of the combined luteolin-astragaloside IV treatment was administered directly at the site of the injury. The animals were then carefully monitored over a five-week period, during which their motor functions were evaluated using a battery of standardized behavioral assessments. The outcomes were striking and statistically significant. The animals that received the combination therapy demonstrated substantial and progressive improvements in their motor capabilities, regaining a degree of mobility that was notably superior to that of the control groups. These functional gains underscored the therapeutic potential of the drug pair in a living organism, translating the protective effects seen in a petri dish into tangible physical recovery.
The observed functional recovery was not merely a transient effect but a sustained improvement that progressed throughout the five-week observation window, suggesting that the therapy was not just temporarily masking symptoms but was facilitating genuine, underlying tissue repair. The detailed behavioral assessments, which measure everything from limb movement to coordinated walking, provided quantitative evidence that the treatment was restoring complex motor pathways. This is a critical finding, as many experimental therapies show initial promise but fail to deliver lasting functional benefits. The success of a single, localized dose also carries significant clinical implications, suggesting a treatment protocol that could be less invasive and carry a lower risk of systemic side effects compared to long-term, systemic drug administration. The consistency and magnitude of the recovery in the treated group provided a powerful validation of the synergistic strategy, confirming its efficacy in a complex biological system that closely mimics human SCI.
Evidence of Physical Tissue Repair
The remarkable functional gains observed in the treated animal models were strongly corroborated by compelling evidence of physical repair at the tissue level. Following the five-week study period, a detailed histological analysis was performed on the injured spinal cords, revealing profound structural differences between the treated and control groups. The examination showed that the combination therapy led to a significant reduction in tissue cavitation, which is the formation of destructive, empty cavities within the spinal cord that permanently disrupts neural circuitry. Furthermore, the animals that received the luteolin-astragaloside IV treatment presented with a substantially smaller overall lesion area. This reduction in the physical footprint of the injury was accompanied by an enhanced structural integrity of the spinal cord tissue itself, indicating that the therapy had effectively preserved more of the vital neural architecture. These microscopic findings provided a direct physical explanation for the macroscopic functional improvements seen in the behavioral tests.
The preservation of tissue integrity is a crucial element in promoting recovery, as it provides a more stable and supportive scaffold for any potential axonal regeneration to occur. The therapy’s ability to limit the spread of the lesion and reduce cavitation suggests that it effectively interrupts the secondary injury cascade that typically continues to destroy tissue for weeks or even months after the initial trauma. By creating a less damaged and more organized tissue environment, the treatment lays the groundwork for endogenous repair mechanisms to function more effectively. The histological data, therefore, did more than just confirm the behavioral results; it offered a window into how the recovery was happening at a structural level. It showed that the drug pair was not just protecting cells from death but was actively mitigating the large-scale tissue destruction that is a hallmark of severe spinal cord injury, a finding that significantly strengthens the case for its therapeutic potential.
Uncovering the Mechanisms of Action
Taming the Inflammatory Response
To delve deeper into the biological mechanisms driving these impressive results, the researchers conducted a detailed molecular and cellular analysis of the repaired tissue. Their findings revealed that the combined treatment effectively suppressed the excessive activation of microglia and astrocytes. In the context of SCI, these glial cells are the primary orchestrators of the powerful and often destructive post-injury inflammatory response. When over-activated, they release a barrage of inflammatory molecules that can kill surviving neurons and, crucially, they coalesce to form the glial scar. This dense scar tissue acts as both a physical and a chemical barrier that actively blocks nerve fibers from regenerating and reconnecting across the injury site. By taming this aggressive glial response, the luteolin-astragaloside IV therapy helped to create a far more permissive and pro-regenerative environment within the injured spinal cord, dismantling one of the most significant obstacles to natural repair.
The modulation of the glial response is a sophisticated process that goes beyond simple anti-inflammatory action. Instead of indiscriminately wiping out these cells, which also have some beneficial roles, the therapy appeared to guide them away from their chronic, destructive state toward a more pro-repair phenotype. This nuanced control is essential for achieving a positive therapeutic outcome. By downregulating the signals that lead to scar formation, the treatment allows for the potential regrowth of axons and the migration of other beneficial cells to the injury site. This controlled calming of the neuroinflammatory storm is a key reason for the therapy’s success, as it addresses a central pathological feature that has derailed many previous therapeutic attempts. The ability to transform the post-injury microenvironment from a hostile, inhibitory state to one that supports healing is a testament to the power of the synergistic, multi-target approach employed in this study.
Promoting Nerve Fiber Regeneration
In concert with its anti-inflammatory effects, the combination therapy was found to actively promote the preservation and regeneration of crucial neural pathways. Molecular analysis of the tissue showed a significant increase in the presence of neurofilament-positive nerve fibers within and around the lesion site in the treated animals. Neurofilaments are the structural proteins that form the cytoskeleton of axons, and their increased presence is a widely accepted indicator of enhanced axonal survival and regeneration. This finding demonstrates that the treatment does more than just protect the spinal cord from further damage; it actively supports the rebuilding of the very connections that were severed by the injury. This pro-regenerative effect is a critical component of meaningful functional recovery, as simply reducing the lesion size is not enough if the communication lines of the nervous system are not restored.
Furthermore, the therapy was specifically shown to promote the restoration of serotonin-related neural pathways. These descending pathways, which originate in the brainstem, are critically important for the control of motor function, and their disruption is a major contributor to paralysis after SCI. The observed increase in serotonergic fibers in the treated group provides a direct molecular link between the drug’s action and the improved motor outcomes seen in the behavioral tests. It suggests that the drug pair helps to re-establish vital command signals from the brain to the spinal cord circuits below the injury. This dual action of both suppressing inhibitory factors like the glial scar and actively promoting the growth of essential nerve fibers like serotonergic axons illustrates the comprehensive nature of the therapy’s mechanism, highlighting how it fosters a holistic repair process that addresses multiple facets of the injury at once.
A Multi-Target and Complementary Strategy
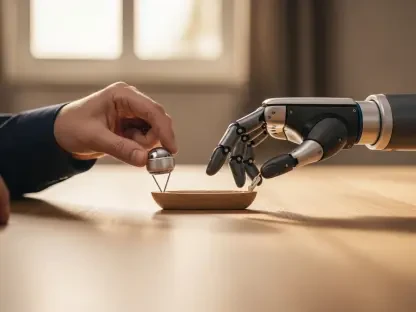
The profound efficacy of the luteolin-astragaloside IV combination stems from its ability to engage multiple molecular targets simultaneously, a conclusion supported by advanced computational network pharmacology and molecular docking analyses. These sophisticated techniques revealed that the two compounds likely act on a complex web of interconnected biological pathways involved in regulating oxidative stress, controlling inflammation, and inhibiting apoptosis. This multi-target action confirms that the therapy’s success is not due to a single, isolated effect but rather its capacity to holistically reshape the entire post-injury microenvironment. As one of the study’s senior authors emphasized, spinal cord injury is not driven by a single pathological process, making it highly unlikely that a single-target drug could ever achieve meaningful recovery. The study underscores the necessity of a more comprehensive therapeutic vision.
The true strength of this strategy lies in the complementary nature of the two compounds. The researchers explained that luteolin is a potent agent against oxidative stress, while astragaloside IV provides robust neural protection and supports regenerative processes. By working in concert, they create conditions that are far more favorable for repair than either compound could achieve on its own. One compound effectively quenches the immediate fire of oxidative damage, while the other begins the work of rebuilding and protecting the neural architecture. This division of labor allows for a coordinated and highly effective response to the injury cascade. This study provides a powerful and well-supported rationale for the continued exploration of synergistic, multi-component therapies for treating complex neurological injuries, shifting the focus from finding a single “magic bullet” to designing a strategic, multi-pronged assault on the disease process.
A New Path for Neurological Therapies
The insights gained from this research have provided a robust framework that could fundamentally reshape the future design of therapies for spinal cord injury. By unequivocally demonstrating that a carefully selected drug pair can produce superior outcomes compared to single-agent treatments, the study championed a necessary paradigm shift toward multi-target strategies for complex neurological repair. Although these results were generated in preclinical models, they established a critical and compelling foundation for the development of safer and more effective combination therapies for human patients. Such treatments showed the potential to reduce the clinical reliance on high-dose steroids, which are often associated with significant side effects, and could offer an alternative to more invasive interventions. The principles of this synergistic approach were also seen as highly relevant beyond spinal cord injury. They could inform innovative treatment strategies for a wide range of other neurodegenerative and traumatic conditions where oxidative stress and inflammation are central pathological features, such as traumatic brain injury, Alzheimer’s disease, and Parkinson’s disease, thereby heralding significant advancements across the broader fields of regenerative and precision medicine.