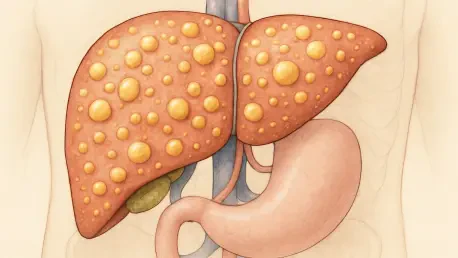
Steatotic liver disease (SLD), encompassing conditions like metabolic dysfunction-associated steatotic liver disease (MASLD), alcohol-related liver disease (ALD), and their overlap (MetALD), has emerged as a dominant global health concern, affecting over 30% of adults worldwide. With its alarming progression to hepatocellular carcinoma (HCC), a deadly form of liver cancer, the urgency to understand and combat this epidemic cannot be overstated. This roundup gathers diverse perspectives from researchers, clinicians, and public health experts to explore the causes, mechanisms, and therapeutic frontiers of SLD. By synthesizing these insights, the aim is to illuminate the multifaceted nature of this disease and highlight actionable strategies for prevention and treatment.
Exploring the Global Burden and Risk Factors
The consensus among health professionals is clear: SLD represents a critical public health challenge, surpassing viral hepatitis as the leading cause of chronic liver issues. Experts emphasize that the skyrocketing prevalence ties directly to modern lifestyle trends, particularly obesity and sedentary habits, which fuel MASLD. Alongside this, excessive alcohol consumption remains a significant driver, contributing to ALD in a vast majority of cases. Many in the field note that the interplay of these factors often results in MetALD, blurring the lines between metabolic and alcohol-related damage.
Differing views emerge on the weight of genetic versus environmental influences. Some researchers argue that genetic variants, such as PNPLA3 and TM6SF2, play a pivotal role in predisposing individuals to fat accumulation in the liver, creating a foundation for disease even in the absence of lifestyle risks. Others counter that while genetics set the stage, environmental factors like diet and alcohol use are the primary accelerators, pointing to data showing heavy drinking linked to 90–95% of SLD cases. This debate underscores a broader call for integrated risk assessment tools that account for both inherited and acquired factors.
Public health advocates also highlight regional disparities in SLD prevalence and risk. In wealthier nations, metabolic drivers like insulin resistance dominate, while in areas with high alcohol consumption, ALD takes precedence. These variations suggest that a one-size-fits-all approach to prevention may fall short, prompting discussions on tailored interventions. The collective insight here is a pressing need to address SLD as a systemic issue, beyond just a liver condition, to curb its global impact.
Unpacking Cellular Mechanisms and Disease Progression
Genetic Predispositions Under Scrutiny
Diving into the cellular and genetic underpinnings, many in the scientific community point to specific mutations as key contributors to SLD susceptibility. Variants like PNPLA3 (I148M) and TM6SF2 (E167K) are frequently cited for their role in disrupting lipid metabolism, leading to hepatic fat buildup. These genetic markers, according to numerous studies, create a vulnerable baseline that lifestyle factors can exacerbate, amplifying the risk of progression.
A contrasting perspective focuses on the limitations of genetic determinism. Some experts caution against overemphasizing inherited risks, noting that not all carriers of these variants develop severe disease. They argue that the interaction with external stressors, such as poor diet or alcohol intake, often determines outcomes, suggesting that genetic screening alone may not predict progression accurately. This viewpoint pushes for broader research into how these interactions unfold over time.
The discussion also touches on the potential of genetic insights for personalized medicine. Enthusiasts in the field advocate for using genetic profiles to identify high-risk individuals early, enabling targeted preventive measures. While promising, this approach faces skepticism from those who highlight the ethical and accessibility challenges of widespread genetic testing, urging a balance between innovation and equity in healthcare applications.
Cellular Dynamics Fueling Liver Damage
At the cellular level, insights reveal a complex battlefield within the liver, where hepatocytes, immune cells like Kupffer cells, and hepatic stellate cells drive inflammation and scarring. Many researchers describe how pathways such as IL-6–STAT3 and TGF-β perpetuate a cycle of damage, transforming mild steatosis into severe fibrosis. This intricate interplay is seen as a core challenge in halting disease advancement.
Differences arise when comparing MASLD and ALD at the cellular scale. Experts focusing on ALD often highlight unique mechanisms, such as acetaldehyde toxicity, which intensifies oxidative stress and triggers neutrophil infiltration—a hallmark of alcohol-associated hepatitis. In contrast, those studying MASLD emphasize metabolic stress and insulin resistance as primary instigators of inflammation. These distinctions suggest that therapeutic targets may need to vary based on the underlying cause.
A recurring concern among clinicians is the difficulty of interrupting these self-sustaining cellular cycles. While some propose early intervention to prevent immune activation, others note that chronic inflammation often persists despite treatment, pointing to gaps in current understanding. This complexity fuels a call for more detailed studies on cellular interactions to uncover novel points of intervention.
From Chronic Damage to Hepatocellular Carcinoma
The progression from SLD to HCC alarms many in the medical field, with a noted shift in cancer etiology. Experts observe that as viral hepatitis cases decline, metabolic and alcohol-related HCC are on the rise, reflecting broader lifestyle changes. Molecular analyses reveal distinct mutation profiles, such as TP53 in ALD-related HCC versus CTNNB1 in MASLD-associated cases, highlighting the need for etiology-specific approaches.
Opinions vary on the predictability of this transition. Some researchers argue that chronic fibrosis serves as a near-inevitable precursor to cancer, advocating for aggressive monitoring of at-risk patients. Others suggest that not all cases follow a linear path, with factors like immune dysregulation playing unpredictable roles. This uncertainty complicates efforts to standardize screening protocols across diverse populations.
There is also debate over the impact of regional differences in HCC patterns. Specialists from various global regions note that dietary habits and alcohol culture influence cancer prevalence, with some areas seeing faster rises in metabolically driven cases. These observations reinforce the argument for localized strategies in cancer prevention, ensuring that interventions align with specific demographic risks.
Emerging Therapies and Implementation Challenges
On the therapeutic front, optimism abounds with recent advancements like Resmetirom, an FDA-approved drug for MASLD, and GLP-1-based therapies such as tirzepatide, which significantly reduce liver fat. Many clinicians praise these innovations for targeting metabolic and inflammatory pathways directly, offering hope for slowing disease progression. For HCC, combinations like atezolizumab plus bevacizumab are hailed as game-changers in extending survival rates.
However, not all voices are equally enthusiastic about accessibility. Some public health experts warn that these cutting-edge treatments often remain out of reach for underserved populations, exacerbating health disparities. They stress that high costs and limited distribution networks hinder widespread adoption, calling for policies to ensure equitable access to these breakthroughs.
Another point of contention lies in the role of personalized medicine. Proponents argue that tailoring therapies to genetic and molecular profiles could revolutionize outcomes, citing early successes in small cohorts. Critics, however, question the scalability of such approaches, noting the lack of infrastructure in many healthcare systems to support individualized care. This divide highlights a broader need for systemic improvements alongside scientific progress.
Key Takeaways and Practical Guidance
Synthesizing these diverse perspectives, it becomes evident that SLD stands as a global health priority, driven by a mix of genetic, cellular, and lifestyle factors. The insights gathered reveal a shared understanding of the disease’s complexity, from its cellular mechanisms to its potential culmination in HCC. Targeted therapies, while promising, must be matched with efforts to address underlying risks through lifestyle changes.
Practical steps forward include prioritizing weight management and alcohol reduction as first-line defenses against SLD. Health professionals across the board advocate for public education campaigns to raise awareness of these modifiable factors. Additionally, there is strong support for integrating genetic screening into routine care to identify vulnerable individuals early, allowing for proactive monitoring.
Beyond individual actions, the roundup points to the importance of systemic change. Experts collectively urge policymakers to invest in research and infrastructure to make advanced therapies more accessible. By blending personal responsibility with broader public health initiatives, there is potential to mitigate the burden of SLD and its deadly consequences.
Reflecting on the Path Ahead
Looking back on the discussions, the depth of insight into steatotic liver disease provides a critical lens on a pressing health crisis. The varied opinions underscored the intricate balance of genetic predisposition, environmental triggers, and cellular dynamics in shaping disease outcomes. Therapeutic advancements stood out as beacons of hope, tempered by the stark reality of access challenges.
Moving forward, a dual focus on prevention and innovation offers a promising roadmap. Stakeholders should consider amplifying efforts in community-based programs that promote healthier lifestyles while also pushing for research into cost-effective treatments. Exploring further resources on liver health and cancer prevention could deepen understanding and inspire actionable change in this ongoing battle against SLD and its complications.