What if a single puff of cigarette smoke could turn the body’s own defenses into a weapon for one of the deadliest cancers? Pancreatic cancer, a disease with a grim five-year survival rate of just 12%, claims over 60,000 new victims annually in the U.S. alone, and for smokers, the danger skyrockets—not just in risk but in the sheer aggression of the disease. Groundbreaking research has unveiled a chilling mechanism: cigarette toxins don’t merely trigger tumors; they hijack the immune system to supercharge cancer’s spread. This discovery sets the stage for a deeper look into how a common habit fuels a silent killer.
Why This Link Is Critical
Pancreatic cancer stands as a ruthless adversary, often diagnosed too late for effective treatment. For smokers, the stakes are even higher—data shows they face up to double the risk of developing this disease compared to nonsmokers. Beyond initial odds, smoking accelerates tumor growth and worsens outcomes, painting a dire picture for millions globally who still light up. This connection isn’t just a statistic; it’s a call to unravel how deeply cigarette toxins manipulate the body’s natural safeguards, pushing an already lethal cancer into overdrive.
Understanding this link carries immense weight for public health. With smoking remaining a pervasive habit, the urgency to address its role in pancreatic cancer cannot be overstated. Insights into this deadly interplay could transform prevention strategies, refine screening protocols, and inspire new treatments tailored to those most at risk. The fight against this cancer demands attention to every factor that fuels it, especially one as preventable as smoking.
Decoding the Science Behind the Damage
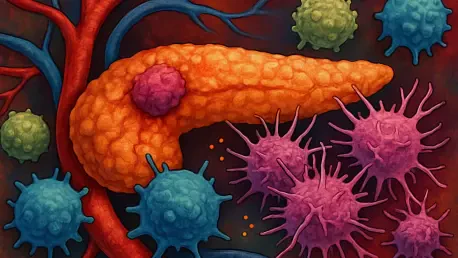
At the heart of this alarming connection lies a sinister process: cigarette smoke rewires the immune system to aid cancer’s advance. Research reveals that toxins in smoke act as catalysts, causing pancreatic tumors in experimental models to grow larger and spread faster than in unexposed conditions. These chemicals don’t just damage tissue; they create a biological environment where cancer thrives unchecked, exploiting the body’s own mechanisms.
A key player in this process is a protein known as Interleukin-22 (IL-22), released by immune cells when exposed to cigarette toxins. This protein binds to specific receptors, altering the tumor’s surroundings to favor rapid growth and metastasis. It’s a devastating betrayal—IL-22, meant to regulate immune responses, becomes a fuel for cancer’s aggression under the influence of smoke, highlighting the profound disruption caused by these toxins.
Perhaps most striking is the role of T-regulatory cells (Tregs), a subset of immune cells that turn traitor in this scenario. Not only do they produce IL-22, but they also suppress the body’s anti-tumor defenses, effectively disarming the immune system. Studies show elevated Treg levels in smokers with pancreatic cancer, underscoring how smoking transforms protectors into accomplices, crippling the fight against this relentless disease.
Expert Voices Shed Light on the Crisis
Researchers driving this discovery emphasize its stark implications. “Cigarette toxins directly reshape the immune landscape, crafting a haven for pancreatic cancer to flourish,” notes a lead investigator involved in the study. This insight isn’t confined to lab results—clinical observations confirm higher Treg levels in smoker patients, mirroring experimental findings and painting a grim reality for those affected.
On the front lines, oncologists witness the toll firsthand. Smoker patients frequently present with more advanced disease at diagnosis, a trend now explained by immune suppression. This pattern complicates treatment plans, often leaving medical teams with fewer options to combat an already aggressive cancer. The alignment between research and real-world outcomes stresses the need for urgent action to address this compounded risk.
The human cost of these findings cannot be ignored. For patients whose smoking history intertwines with their diagnosis, the prognosis often feels like a double blow. These insights push for a reevaluation of how healthcare systems manage high-risk groups, urging a focus on both prevention and innovative care strategies to counter the immune damage inflicted by cigarette smoke.
Real Stories, Real Impact
Consider the case of a 58-year-old man, a lifelong smoker, diagnosed with pancreatic cancer at a late stage. His doctors noted rapid tumor progression, a hallmark now linked to the immune suppression caused by years of cigarette use. Such stories are not rare—countless patients face similar battles, where smoking history amplifies an already daunting fight, often leaving families grappling with limited time and options.
In clinical settings, these patterns emerge repeatedly. Data indicates that smoker patients often endure poorer responses to standard therapies, a challenge tied to the altered immune environment described in recent studies. This reality frustrates both patients and providers, who must navigate a disease made fiercer by a preventable habit, highlighting the personal stakes behind the science.
Beyond individual cases, the broader impact on communities is staggering. With smoking still prevalent in many regions, entire populations face heightened risks of aggressive pancreatic cancer. These stories fuel the urgency to translate research into action, ensuring that knowledge of immune suppression leads to tangible improvements in care and awareness for those most vulnerable.
Steps to Break the Deadly Cycle
Armed with this understanding, actionable measures can help curb the devastating link between smoking and pancreatic cancer. The first and most critical step is cessation—quitting smoking can halt the immune suppression that drives tumor growth. Resources like counseling and nicotine replacement therapies offer vital support, especially for those with a family history of the disease, where risks are already elevated.
Awareness of early warning signs also plays a pivotal role. Smokers should monitor for symptoms such as persistent low back pain, jaundice, or sudden weight loss, which could signal pancreatic cancer. Reporting these to a healthcare provider promptly may improve the chances of early detection, a crucial factor in a disease often caught too late for effective intervention.
Advocacy for tailored screening and research funding rounds out the fight. Smokers should discuss enhanced screening options with their doctors, while supporting clinical trials targeting immune pathways offers hope for new therapies. Inhibiting Treg activity or toxin-driven mechanisms has shown promise in shrinking tumors, a breakthrough that could revolutionize treatment if developed further. These steps empower individuals and systems alike to confront the unique challenges posed by smoking-related immune damage in pancreatic cancer.
Reflecting on a Path Forward
Looking back, the journey to uncover how smoking fueled pancreatic cancer through immune suppression revealed a harrowing truth about the body’s betrayal under the influence of cigarette toxins. The identification of IL-22 and T-regulatory cells as key culprits provided a critical lens into the aggression of this disease among smokers. Each finding built a clearer picture of why outcomes were so dire for those with this habit.
The stories of patients, burdened by advanced diagnoses linked to their smoking history, added a human dimension to the stark data. Clinicians, too, faced the frustration of battling a cancer made fiercer by preventable factors. These experiences underscored the weight of translating scientific breakthroughs into real-world impact, a mission that gained momentum with every revelation.
Moving ahead, the focus must shift to empowering change—encouraging cessation, enhancing symptom awareness, and pushing for therapies that target the immune damage caused by smoke. Collaboration between researchers, healthcare providers, and communities holds the key to turning these insights into lives saved. The path is challenging, but with sustained effort, the grip of this deadly connection can be loosened, offering hope where once there was only despair.