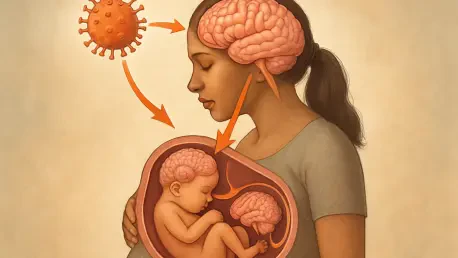
The intersection of severe influenza during pregnancy and its potential to harm fetal brain development has emerged as a critical concern for both expectant mothers and medical professionals, prompting urgent attention. A pioneering study conducted by researchers at the University of Illinois Urbana-Champaign, published in Brain, Behavior, and Immunity, sheds light on this alarming issue through experiments on pregnant mice. By exposing subjects to live influenza virus to replicate real-world infections, the findings reveal how severe flu can breach vital protective barriers, allowing harmful molecules to infiltrate the fetal brain. This breach poses significant risks to neurodevelopment, with implications that may extend to human health. As flu season approaches each year, understanding these dangers becomes paramount, highlighting the need for preventive strategies to protect vulnerable populations during pregnancy.
Unveiling the Dangers of Maternal Influenza
Compromising Critical Protective Barriers
The protective barriers of the placenta and fetal brain serve as essential defenses for a developing fetus, yet severe influenza can drastically undermine their integrity. Research demonstrates that in cases of intense infection, these barriers become permeable, allowing harmful substances to seep into fetal tissues. Unlike milder infections where these defenses typically remain intact, severe flu creates a dangerous pathway for molecular infiltration. Notably, large tracers, which an intact blood-brain barrier would normally block, were found accumulating in the fetal brain of affected mice. This “leakiness” signals a profound vulnerability during critical stages of development, raising concerns about the potential for lasting damage when a pregnant individual contracts a severe case of the flu.
The implications of this barrier breakdown extend beyond immediate physical effects, pointing to a deeper systemic issue during severe maternal infections. The placenta, often overlooked in developmental studies, plays a pivotal role in shielding the fetus from external threats. When influenza reaches a critical severity, this protective function falters, exposing the fetus to toxins and inflammatory agents that should never cross into its environment. Such findings underscore the importance of infection severity as a determining factor in fetal risk. The research aligns with human epidemiological data suggesting that while not all maternal flu cases pose a threat, the more severe the illness, the greater the potential harm to the developing child, emphasizing the urgency of addressing this issue.
Tracing Harmful Molecular Infiltration
Beyond the initial breach of protective barriers, the infiltration of specific harmful molecules into the fetal brain presents a dire threat during severe influenza infections. The study highlights the accumulation of large molecular tracers in the fetal brain, substances that an intact barrier would typically repel. Alongside these tracers, fibrinogen—a molecule associated with blood clotting but damaging when present in the brain—was detected in significant amounts. This presence suggests an inflammatory state that could disrupt the delicate balance of brain development, potentially leading to neuronal damage or altered growth patterns in affected regions.
Further exploration into this molecular invasion reveals its targeted impact on critical areas of the fetal brain, such as the subventricular zone and choroid plexus. These regions are vital for the formation and differentiation of neurons, and their exposure to harmful substances during severe maternal flu can create an oxidative environment conducive to cell death. The study’s use of live influenza virus at varying doses provides a realistic simulation of seasonal flu, showing that only severe cases trigger such profound effects. This threshold of severity offers a nuanced understanding of risk, indicating that the extent of molecular infiltration directly correlates with the intensity of the infection, a finding that mirrors patterns observed in human health data.
Strategies to Safeguard Fetal Health
Emphasizing the Role of Vaccination
In light of the risks posed by severe influenza during pregnancy, preventive measures take on heightened importance, with vaccination standing out as a cornerstone of protection. The research strongly advocates for flu shots among pregnant individuals as a means to significantly reduce the likelihood of severe infections. By bolstering immunity, vaccines help preserve the integrity of both placental and fetal brain barriers, preventing the dangerous infiltration of harmful molecules. This protective effect is crucial during flu season, when the risk of exposure spikes, and aligns with broader public health recommendations that prioritize maternal immunization to safeguard fetal development.
Moreover, the impact of vaccination extends beyond individual protection, contributing to community-wide efforts to curb flu transmission. The study’s findings resonate with human data indicating that the severity of maternal infection often dictates the degree of risk to the fetus. By mitigating the chances of severe illness, vaccines offer a proactive solution to a problem that could otherwise lead to long-term neurodevelopmental challenges. Public health campaigns must therefore focus on raising awareness about the benefits of flu shots during pregnancy, ensuring that expectant mothers have access to this critical intervention to protect both themselves and their unborn children from the devastating effects of severe influenza.
Addressing Long-Term Neurodevelopmental Concerns
The potential long-term consequences of severe maternal flu on fetal brain development cannot be overstated, as the infiltration of harmful substances may alter critical growth trajectories. Affected brain regions, essential for neuronal differentiation, face disruption when exposed to inflammatory and oxidative conditions triggered by severe infections. Such disruptions could manifest as cognitive or mental health challenges later in life, a concern that the research brings to the forefront. Understanding these risks provides a foundation for developing targeted interventions that address not only immediate threats but also future developmental outcomes for children exposed to severe maternal influenza.
Equally important is the need for ongoing research to fully grasp the scope of these neurodevelopmental impacts and refine preventive strategies accordingly. The study’s focus on live virus exposure offers a realistic model for human scenarios, suggesting that severe flu cases pose a tangible threat to long-term brain health. Healthcare providers should integrate these insights into prenatal care, emphasizing education about flu prevention and the importance of early intervention. As science continues to uncover the intricate links between maternal health and fetal outcomes, a multifaceted approach—combining vaccination, awareness, and advanced research—remains essential to mitigate risks and ensure healthier futures for the next generation.