The relentless pursuit of effective chronic pain management has led millions of people down a path lined with cannabis products, each promising a definitive end to their suffering. As legalization expands and access grows, cannabis has transitioned from a fringe substance to a mainstream wellness product, frequently positioned as a natural and powerful alternative to conventional pharmaceuticals. This review serves to cut through the anecdotal claims and marketing fervor, offering a clear-eyed evaluation of the scientific evidence to determine whether cannabis truly holds the key to lasting pain relief.
Evaluating the Evidence: Is Cannabis a Viable Solution for Chronic Pain?
The modern marketplace is saturated with cannabis-based options, from oils and edibles to tinctures and topical creams, all promoted as remedies for chronic pain. This proliferation is largely driven by compelling personal stories and a cultural shift toward plant-based medicine, creating a powerful perception of efficacy. The critical question, however, is whether this widespread public acceptance is supported by rigorous clinical data. A careful examination of the evidence is essential to separate legitimate therapeutic potential from wishful thinking.
Answering this question is complicated by the inherent variability of cannabis itself. Unlike a standardized medication with a precise dosage and chemical composition, cannabis products are notoriously inconsistent. The effects can differ dramatically based on the plant strain, cultivation methods, and extraction processes used. This lack of uniformity makes it incredibly challenging for researchers to conduct definitive studies and for consumers to find a reliable, repeatable experience, turning the search for pain relief into a frustrating process of trial and error.
Understanding the Key Compounds: THC vs. CBD in Pain Management
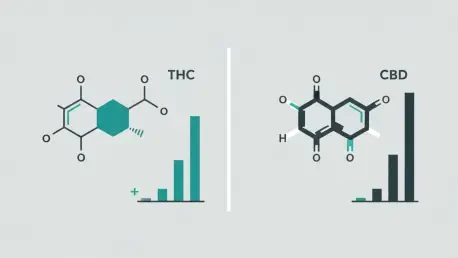
At the heart of any discussion about cannabis are its two primary active compounds: tetrahydrocannabinol (THC) and cannabidiol (CBD). THC is the well-known psychoactive component responsible for the “high” associated with marijuana use. In contrast, CBD is marketed as its non-intoxicating counterpart, celebrated for its purported therapeutic benefits without the euphoric effects. Consumers are often led to believe that these compounds can be used interchangeably or that CBD is the superior medicinal choice, but their roles in pain management are fundamentally different.
Recent systematic reviews of clinical trials have begun to challenge the popular narrative surrounding these two cannabinoids. While CBD has been widely embraced as a powerful, non-psychoactive analgesic, the evidence supporting this claim is surprisingly weak. The latest research indicates that products containing mainly or exclusively CBD show almost no measurable improvement in chronic pain. Instead, the data consistently points toward THC as the compound responsible for the modest pain-relieving effects observed in studies, a finding that directly contradicts the conventional wisdom guiding many consumers.
Clinical Effectiveness and Side Effect Profile
A closer look at the data reveals that cannabis products with relatively high concentrations of THC can offer a small, short-term improvement in pain levels. This finding holds true for both plant-derived products and synthetic THC medications available by prescription, such as dronabinol and nabilone. However, the degree of relief is modest at best. On a standard 10-point pain scale, the improvement is typically only about half a point to one point better than a placebo, an effect that may be statistically significant but not always clinically meaningful for someone suffering from severe, persistent pain.
This marginal benefit is further tempered by a considerable list of potential side effects. The use of high-THC products is consistently linked to a moderate-to-large increase in the risk of experiencing adverse events. The most common among these are dizziness, sedation, and nausea, which can impair daily functioning and quality of life. This trade-off between a slight reduction in pain and the likelihood of developing disruptive side effects is a crucial factor that must be weighed by anyone considering cannabis for therapeutic purposes.
Balancing Modest Benefits Against Significant Risks
The decision to use cannabis for chronic pain ultimately hinges on a delicate risk-benefit analysis. For an individual whose life is severely limited by pain, a half-point reduction on the pain scale might feel like a worthwhile gain, even if it comes with dizziness or fatigue. For others, the same side effects could be intolerable, making the modest analgesic effect an insufficient reward. This personal calculation is at the core of the debate and explains why experiences with medical cannabis are so varied.
This ambiguity is reflected in the divided stance of the medical community. Major organizations like the American College of Physicians have recently declined to recommend inhaled cannabis for non-cancer pain, citing insufficient evidence and potential harms. Meanwhile, other expert panels have issued cautious endorsements for its use, but typically only as a last resort for patients who have not found relief from standard, evidence-based treatments. This lack of consensus underscores the fact that cannabis is not yet a well-understood or universally accepted medical tool.
Synthesizing the OHSU Review: A Verdict on THC and CBD
When all the evidence is synthesized, a clear verdict on the two main cannabinoids begins to emerge. THC offers a slight but measurable therapeutic advantage for short-term pain relief. However, this benefit is inextricably linked to its psychoactive nature and a significant risk of undesirable side effects. Therefore, it cannot be considered a first-line treatment, but it remains a potential option for specific cases where other therapies have failed.
The verdict on CBD, at least for now, is far more definitive and perhaps disappointing for many. Despite its immense popularity and the marketing that portrays it as a cure-all, the current body of high-quality evidence from randomized controlled trials shows it to be ineffective for managing chronic pain. This conclusion is a critical reality check for a market saturated with products that promise relief based on little more than anecdotal reports and clever branding.
Informed Decisions and the Path Forward for Research
The primary purpose of evaluating this clinical evidence is to empower patients and consumers to make more educated decisions. By understanding that THC’s benefits are modest and come with significant caveats, while CBD’s pain-relieving properties appear to be negligible, individuals can approach the crowded cannabis market with healthy skepticism. This knowledge provides a foundation for more productive conversations with healthcare providers about whether cannabis is a reasonable addition to a comprehensive pain management plan.
Ultimately, the current body of research illuminates just how much remains unknown. There is a pressing need for more rigorous, long-term studies to assess the safety and efficacy of sustained cannabis use. Future research must also compare the effectiveness of different formulations and delivery methods—such as oral versus inhaled products—and work to understand how findings from controlled trials apply to the complex, varied products available in dispensaries. This continued scientific inquiry is the only path toward unlocking the true therapeutic potential of cannabis and establishing its proper place in modern medicine.