In the vast landscape of medical diagnostics, few challenges are as perplexing as identifying rare cancers that mimic more common diseases, such as primary pancreatic lymphoma (PPL), which accounts for less than 1% of all pancreatic cancers. Hodgkin lymphoma in this location is an even rarer anomaly, often leading to misdiagnosis because its symptoms and imaging closely resemble the far more prevalent pancreatic adenocarcinoma. This roundup article delves into the complexities of diagnosing and treating pancreatic Hodgkin lymphoma, gathering insights, opinions, and tips from various medical perspectives to illuminate this diagnostic conundrum. The purpose is to provide clinicians and researchers with a comprehensive view of current challenges and strategies, fostering a deeper understanding of how to approach such uncommon cases.
Diverse Perspectives on a Hidden Challenge
Unpacking the Rarity and Diagnostic Difficulty
Across the medical community, there is a consensus that pancreatic Hodgkin lymphoma represents an exceptional diagnostic hurdle due to its infrequent occurrence outside typical lymphatic regions. Hematologists have noted that the pancreas as an extranodal site for this blood cancer defies conventional expectations, often leading to initial assumptions of more common malignancies. This rarity means that many practitioners may never encounter such a case in their careers, underscoring the need for heightened awareness.
Varied opinions emerge on how best to integrate this awareness into routine practice. Some oncologists advocate for educational initiatives that emphasize atypical presentations in medical training, arguing that early exposure to rare cases can sharpen diagnostic skills. Others suggest that clinical guidelines should include mandatory consideration of rare differentials for pancreatic masses, ensuring that no possibility is overlooked during patient evaluations.
Symptoms That Mislead: A Common Thread
A recurring observation from gastroenterologists and oncologists alike is the deceptive nature of symptoms associated with pancreatic Hodgkin lymphoma. Fever, abdominal pain, and unintentional weight loss are frequently reported, mirroring the clinical picture of adenocarcinoma. This overlap often delays accurate diagnosis, as clinicians may lean toward the more probable condition based on prevalence alone.
Diagnostic radiologists add another layer to this discussion, highlighting that imaging techniques such as CT scans or MRIs often reveal a pancreatic mass indistinguishable from more common tumors. Many in the field stress the importance of not stopping at imaging, pushing for further investigation even when results seem conclusive. This shared viewpoint underscores a critical need for skepticism in the face of seemingly straightforward findings.
Diagnostic Strategies: A Range of Expert Tips
The Pivotal Role of Biopsy Over Imaging
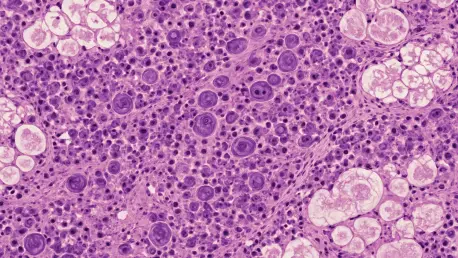
One of the most consistent recommendations from pathologists and oncologists is the indispensable role of biopsy in confirming a diagnosis of pancreatic Hodgkin lymphoma. Unlike adenocarcinomas, lymphomas rarely cause tissue necrosis or duct obstruction, a subtlety that imaging alone cannot reliably detect. Experts widely agree that invasive diagnostics are non-negotiable in cases where imaging is inconclusive or suggests a common malignancy.
Some specialists emphasize the importance of specific staining techniques during biopsy analysis to identify subtypes like nodular sclerosis, which can significantly alter treatment plans. A practical tip often shared is to ensure close collaboration with pathology teams to expedite results, minimizing delays in initiating appropriate therapies. This approach is seen as a cornerstone of tackling rare cancers effectively.
Broadening Differential Diagnoses
Another key insight from medical professionals is the necessity of expanding differential diagnoses beyond the usual suspects when evaluating pancreatic masses. Many clinicians argue that the default assumption of adenocarcinoma can be a dangerous oversight, particularly in atypical presentations. This perspective calls for a cultural shift in diagnostic thinking, urging practitioners to consider rare entities like PPL.
Differing views exist on how to implement this shift practically. Some suggest integrating decision-support tools into electronic health records to prompt consideration of uncommon conditions. Others believe that case-based learning, where rare presentations are discussed in detail during medical rounds, can better prepare teams to recognize outliers in real-world scenarios.
Treatment Approaches: Tailored Solutions in Focus
Shifting Paradigms with Targeted Therapies
On the treatment front, there is broad agreement among hematologists that accurate diagnosis of pancreatic Hodgkin lymphoma paves the way for tailored therapies like the A+AVD chemotherapy regimen. This approach starkly contrasts with treatments for adenocarcinoma, such as surgery or radiation, highlighting the transformative impact of precise identification. Many experts view this as a testament to the value of personalized medicine in rare cancer management.
Emerging opinions also point to the potential of novel agents like brentuximab vedotin, which have shown promise in Hodgkin lymphoma cases. Some researchers advocate for clinical trials to further explore these therapies in extranodal presentations, believing that innovation could redefine outcomes. This forward-looking stance reflects a collective optimism about refining treatment protocols over time.
Interdisciplinary Collaboration as a Key Strategy
A frequently cited tip from treatment specialists is the importance of interdisciplinary collaboration in managing such rare cases. Oncologists, pathologists, and radiologists must work in tandem to align diagnostic findings with therapeutic strategies. This collaborative model is often praised for its ability to reduce errors and optimize patient care.
Slight variations in opinion exist regarding how to structure these collaborations. Certain professionals recommend regular multidisciplinary tumor boards to discuss complex cases, ensuring all perspectives are considered. Others suggest leveraging digital platforms for real-time consultations, especially in settings where in-person meetings are challenging, to maintain continuity in decision-making processes.
Reflecting on Shared Wisdom and Next Steps
Looking back, this exploration of pancreatic Hodgkin lymphoma through diverse medical lenses revealed a unified concern about diagnostic oversight due to its rarity and deceptive presentation. The insights gathered underscored a collective push for biopsy-driven diagnostics, broader differential considerations, and tailored therapeutic approaches. Varied strategies, from educational reforms to interdisciplinary teamwork, highlighted the multifaceted efforts needed to address this challenge.
Moving forward, clinicians are encouraged to adopt a mindset of curiosity, questioning initial assumptions about pancreatic masses and advocating for thorough investigations. A practical next step involves staying updated on evolving therapies through continuous learning and participation in professional networks focused on rare cancers. Additionally, fostering research into genetic or environmental factors behind such presentations emerged as a vital consideration, promising to enhance understanding and improve patient outcomes in the years ahead.