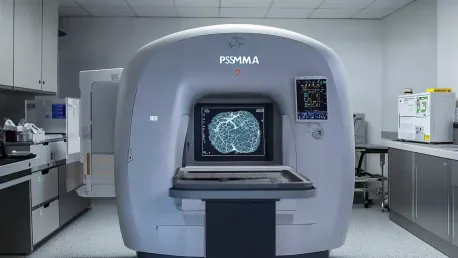
Recent advancements in imaging technology have caused a significant shift in how high-risk nonmetastatic hormone-sensitive prostate cancer is staged. Conventional imaging techniques, which have long been the standard, might have significantly underestimated the extent of metastasis in these patients. Researchers at the UCLA Health Jonsson Comprehensive Cancer Center conducted a study revealing that a considerable proportion of patients initially classified as nonmetastatic actually had metastatic disease when assessed using an advanced imaging technique known as prostate-specific membrane antigen-positron emission tomography (PSMA-PET).
PSMA-PET vs. Conventional Imaging
Underestimation by Conventional Methods
The study, published in JAMA Network Open, underscored the dramatic difference PSMA-PET can make in accurately staging prostate cancer. Nearly 50% of the patients, who were initially deemed to have nonmetastatic high-risk prostate cancer through conventional imaging methods, were found to have metastatic disease when assessed with PSMA-PET. This advanced imaging technology uses radiotracers that specifically bind to prostate cancer cells, offering a more comprehensive view of cancer’s biological activities compared to traditional imaging techniques that only capture anatomical details.
A pivotal finding from this study is that 46% of patients, previously thought to have localized disease based on conventional imaging, were discovered to have hidden metastases through PSMA-PET. More specifically, 24% of these patients had five or more lesions that were missed by conventional imaging methods. These significant percentages highlight how traditional imaging could substantially underestimate the extent of the disease’s spread, potentially impacting treatment decisions and outcomes negatively.
Implications for Treatment Strategies
The insights from this study are critical for the medical community. Senior author Dr. Jeremie Calais stressed that PSMA-PET’s role in accurately staging prostate cancer could substantially influence treatment decisions. Historically, clinical trials and treatment protocols have relied on conventional imaging, which may fail to detect the full extent of disease progression. For example, prior research, such as the EMBARK trial, demonstrated that enzalutamide combined with androgen deprivation therapy improved metastasis-free survival. However, this conclusion was based on patient selections using conventional imaging, likely missing a portion of metastases.
Dr. Adrien Holzgreve, a visiting assistant professor and first author of the study, emphasized the unexpected extent of metastatic findings within the defined patient cohort that traditional imaging considered nonmetastatic. This revelation advocates for the integration of PSMA-PET into patient selection strategies for clinical trials and routine clinical assessments. The improved accuracy of PSMA-PET can lead to more tailored and potentially more effective treatment regimens for patients, challenging and possibly revising longstanding treatment paradigms.
Future Directions and Clinical Integration
Need for Further Research
While the results of the study mark significant advances, the researchers stressed the need for further high-quality prospective data to establish the long-term superiority of PSMA-PET in improving patient outcomes. Future research efforts at UCLA and within the broader medical research community are critical to consolidating the role of PSMA-PET and developing optimized treatment protocols based on its findings.
Ongoing research at UCLA seeks to analyze follow-up data to better understand how PSMA-PET findings influence treatment choices and patient outcomes. As part of an international consortium examining over 6,000 patients, the research aims to explore the prognostic value of PSMA-PET in providing a comprehensive picture of prostate cancer progression. These efforts aim to deliver more robust data to support the clinical integration of PSMA-PET.
A Shift in Clinical Practices
Recent advancements in imaging technology have revolutionized the staging of high-risk nonmetastatic hormone-sensitive prostate cancer. Traditional imaging techniques, long considered the standard, may have greatly underestimated the spread of metastasis in these patients. A study conducted by researchers at the UCLA Health Jonsson Comprehensive Cancer Center unveiled that a significant portion of patients initially believed to be nonmetastatic were, in fact, found to have metastatic disease when assessed using an advanced imaging method known as prostate-specific membrane antigen-positron emission tomography (PSMA-PET). This new imaging technique has proven more accurate in detecting metastasis at an earlier stage, offering a clearer picture of the disease’s spread. As a result, the revised staging from PSMA-PET can lead to more precise and effective treatment plans, potentially improving patient outcomes. The findings underscore the importance of adopting advanced imaging technologies in the diagnostic process to ensure accurate staging and better patient care in prostate cancer management.