A recent clinical trial has successfully demonstrated that treating a rare and aggressive skin cancer with immunotherapy before surgery can completely eliminate tumors in the majority of patients, heralding a profound shift in how this formidable disease is managed. The groundbreaking research, co-led by investigators at the University of California, Los Angeles (UCLA), provides compelling evidence that empowering the body’s own immune system prior to the first incision can spare patients from disfiguring procedures and significantly improve long-term survival rates. This neoadjuvant approach is poised to become the new standard of care, offering durable disease control and a much-improved quality of life.
Could a Treatment Before the First Incision Redefine Cancer Surgery?
The conventional path for treating operable cancers has long followed a strict sequence: surgically remove the tumor, then address any remaining cells with subsequent therapies like radiation. A transformative clinical trial, however, has challenged this established dogma by asking a pivotal question: what if the most potent weapon against cancer is unleashed before a surgeon even enters the operating room? This study investigated that very idea for a rare skin cancer, exploring whether pre-surgical treatment could not only shrink tumors but eradicate them entirely, fundamentally altering patient outcomes.
The research centered on the SWOG S1512 clinical trial, a multicenter effort designed to test the efficacy of immunotherapy administered prior to surgical intervention. Organized by the SWOG Cancer Research Network and funded by the National Cancer Institute, this was the first study of its kind for this specific patient population. By flipping the traditional treatment model on its head, investigators aimed to determine if an immune-based therapy could reduce the extent of surgery required, prevent recurrence, and ultimately establish a safer, more effective standard of care.
Understanding Desmoplastic Melanoma a Formidable Foe
Desmoplastic melanoma is a rare subtype of skin cancer known for its aggressive behavior and clinical complexity. It most often develops on sun-damaged skin, particularly on the head and neck, where it can be challenging to treat surgically without significant cosmetic and functional impact. Unlike more common melanomas that grow superficially, this variant is characterized by its tendency to invade deep into surrounding tissues, creating a firm, scar-like mass that complicates its removal.
What makes this cancer particularly difficult to manage is its propensity for perineural invasion—the ability to grow along nerve pathways. This insidious characteristic increases the risk of local recurrence and makes achieving clean surgical margins a significant challenge. For decades, the standard treatment involved wide and often disfiguring excisions, frequently followed by radiation therapy to control residual disease. Historically, desmoplastic melanoma has also shown a stubborn resistance to systemic treatments like chemotherapy, leaving patients with advanced disease few effective options.
The SWOG S1512 Trial a Paradigm Shift in Action
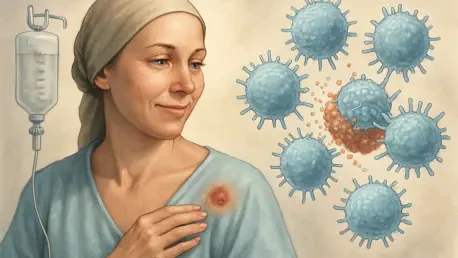
The SWOG S1512 trial was meticulously designed to test a new therapeutic strategy for patients with operable tumors. The study focused on the use of pembrolizumab, an established anti-PD-1 immune checkpoint inhibitor. This class of drug works not by directly attacking cancer cells but by blocking a protein called PD-1, which acts as a brake on the immune system. By inhibiting this protein, pembrolizumab effectively releases the brakes, allowing the body’s T-cells to recognize and mount a powerful assault against the melanoma.
Cohort A of the trial enrolled 28 patients diagnosed with surgically resectable desmoplastic melanoma. These individuals received three cycles of pembrolizumab infusions over a nine-week period leading up to their scheduled operations. To track the treatment’s impact with precision, researchers analyzed tissue samples collected before, during, and after the therapy course. This approach provided a detailed biological picture of how the immunotherapy was activating the immune response and affecting the tumor microenvironment.
Overwhelming Success the Data and Expert Insights
The outcomes of the trial were nothing short of remarkable. An astounding 71% of patients who received the neoadjuvant pembrolizumab achieved a pathologic complete response, meaning that when surgeons removed the tissue where the tumor had been, they found no detectable cancer cells remaining. Furthermore, the treatment was well-tolerated, with most side effects reported as mild, confirming a favorable safety profile for this pre-operative approach.
Dr. Antoni Ribas, a senior author of the study and director of the UCLA Health Jonsson Comprehensive Cancer Center’s Tumor Immunology Program, highlighted the significance of these results. He noted that administering pembrolizumab before surgery proved to be a potent and safe method for reducing the need for extensive surgical procedures. The long-term data reinforced this success. A three-year follow-up revealed a 95% survival rate, and 74% of patients remained completely free of the disease, underscoring the durable efficacy of the treatment.
Forging a New Standard of Care for Patients
The compelling results from the SWOG S1512 trial have positioned pre-surgical immunotherapy as the new clinical benchmark for desmoplastic melanoma. This approach represents a decisive move away from a reliance on repeated, extensive surgeries and follow-up radiation, which carry significant physical and emotional tolls. The study’s findings provide a clear path toward a more effective and less burdensome treatment paradigm.
The tangible benefits for patients are profound. By effectively eliminating the cancer before surgery, this neoadjuvant strategy provides durable disease control, significantly improves survival rates, and enhances quality of life. Patients are more likely to preserve critical functions and avoid the disfigurement associated with large excisions, particularly in sensitive areas like the face and neck. The trial’s success demonstrated a powerful new way to treat this rare cancer, offering a future where therapy is not only more effective but also kinder to the patient.