A fractured bone unleashes an immediate and intense cascade of pain signals, but new evidence compellingly suggests these very same messengers are also the architects of their own repair. For decades, the nervous system’s role in skeletal injury was viewed through a narrow lens: nerves reported damage, and the body’s local cellular machinery handled the cleanup and reconstruction. This perspective is now being fundamentally rewritten. Groundbreaking research reveals a far more intricate and elegant system where the neurons responsible for transmitting pain do not simply act as passive observers. Instead, they function as active commanders, issuing a sophisticated series of molecular orders that directly orchestrate the entire bone healing process from start to finish. This discovery recasts our understanding of regeneration, transforming the very definition of pain from a mere symptom to a critical component of recovery.
More Than a Mouthpiece for Pain What if the Nerves That Signal Injury Are Also in Charge of Fixing It
The traditional view of sensory neurons has long been that of a simple alert system, messengers that do little more than carry a “pain” signal from an injury site to the central nervous system. This new paradigm challenges that belief, introducing the concept that this alert system is deeply integrated with the emergency response it triggers. The nerves are not just reporting the problem; they are actively managing the solution. This represents a significant shift in biological understanding, suggesting a level of neural command over tissue regeneration that was previously unimaginable.
To better visualize this dual function, consider the analogy of a sophisticated smoke alarm. A basic detector simply shrieks when it senses smoke, alerting occupants to the fire. However, the system uncovered in bone repair is far more advanced. These sensory neurons not inly detect the “fire” of a fracture and sound the alarm in the form of pain, but they then transform into a command-and-control center. They actively deploy resources, direct cellular firefighters, and oversee the rebuilding effort, ensuring a coordinated and effective response to the damage.
This revelation effectively dismantles the long-held dogma of pain nerves as passive conduits of information. It repositions them as indispensable commanders in the complex theater of healing. By showing that these neurons possess a pro-regenerative agenda, the research uncovers a hidden layer of biological intelligence. The body, it seems, has co-opted its own warning system to double as a repair crew, an elegant and efficient evolutionary design that ensures the agents closest to the damage are the ones leading the charge to fix it.
The Paradox of Pain and Regeneration Why This Discovery Matters
The intersection of neuroscience and skeletal biology has long been marked by a perplexing question: how can nociceptors, the neurons specifically evolved to transmit signals of severe pain and tissue damage, also play a constructive, pro-regenerative role? This apparent paradox has now been resolved. The research demonstrates that these two functions are not contradictory but are instead two sides of the same coin, representing a dynamic functional shift that occurs over the course of the healing process. This bridges a significant gap in our understanding, showing that the body’s response to injury is a unified process orchestrated by a single, multi-talented neural system.
The clinical implications of this discovery are profound and urgent. Millions of individuals worldwide suffer from impaired or failed bone healing. This is particularly prevalent among the elderly, whose regenerative capacity naturally declines, as well as in patients with systemic conditions like diabetes or peripheral neuropathy, where nerve function is already compromised. For these populations, a simple fracture can lead to chronic pain, disability, and a significant reduction in quality of life. The high incidence of non-unions, where a broken bone fails to heal, underscores the pressing need for novel therapeutic strategies that can enhance the body’s natural repair mechanisms.
This new understanding firmly establishes that fracture repair is not a self-contained, local event driven solely by bone and immune cells. Instead, it is a complex, multi-system process that is heavily dependent on and directed by neural signaling from the peripheral and central nervous systems. The health and function of these command neurons are therefore critical for successful outcomes. This context elevates the nervous system from a secondary player to a central protagonist in the story of skeletal regeneration, opening up entirely new avenues for medical intervention.
Uncovering the Neural Circuitry of Skeletal Healing
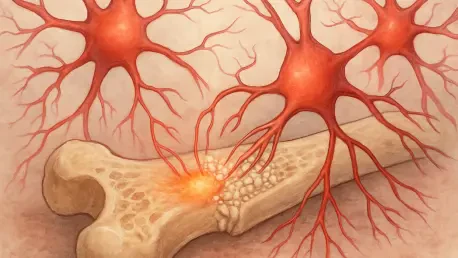
At the heart of this discovery is the meticulous mapping of the direct lines of communication between the nervous system and the skeletal system. Researchers have charted the network connecting peripheral afferent neurons—the nerves that transmit sensory information from the body’s extremities—to the cellular workforce responsible for building new bone. This neural wiring extends directly into the bone tissue, allowing for immediate and precise communication following an injury, ensuring that the nerve’s commands are received directly by the cells tasked with repair.
The function of these dorsal root ganglion (DRG) neurons—the nerve clusters along the spinal cord that house the cell bodies of these sensory nerves—is remarkably dynamic, operating in two distinct phases. In Phase One, immediately after a fracture, the neurons perform their classic role as nociceptors. They generate the perception of pain and initiate a localized inflammatory response, which is crucial for clearing debris and setting the stage for healing. However, this is only the beginning of their mission.
In Phase Two, occurring later in the healing cascade, these same neurons undergo a profound functional transformation. They switch from being alarm-sounders to being master builders, adopting what is described as a “pro-regenerative state.” In this phase, they begin to produce and release a specific cocktail of powerful signaling proteins. This molecular toolkit is designed to orchestrate the complex tasks of reconstruction, including the formation of new blood vessels (angiogenesis), the growth of new nerve fibers into the healing tissue, and, most critically, the development of new bone and cartilage to bridge the fracture gap.
Inside the Research How Scientists Traced the Bodys Repair Commands
The foundational evidence for this neural command system was detailed in a landmark study from Johns Hopkins Medicine, published in the prestigious journal Science. This research provided the first comprehensive map of the neural circuitry governing bone repair, moving the concept from theory to established biological fact. The study built upon earlier work from 2019, which first identified the crucial interaction between nerve growth factor (NGF) and its receptor, TrkA, as essential for drawing nerves into the fracture site and initiating the healing process.
To trace these command pathways, the scientific team employed an innovative methodology centered on retrograde tracing. Using a specially engineered virus with a high affinity for peripheral nerves, they were able to “infect” the nerve endings within the bone. This virus then traveled backward along the nerve fiber—much like following a wire from a light bulb back to the circuit breaker—to label the specific DRG neurons in the spinal cord that innervate the bone. This technique allowed for the precise identification of the exact nerve cells responsible for overseeing skeletal repair.
This mapping was then combined with the powerful technique of single-cell RNA sequencing. By isolating these labeled, bone-innervating neurons from mouse models, both before and after a fracture, researchers analyzed the genetic and protein profiles of each individual cell. This deep dive into their molecular activity created the first-ever single-cell atlas of these specialized neurons, revealing exactly which genes are switched on and which protein signals are released during the healing process. This atlas provides an unprecedentedly detailed schematic of the neural network and its molecular language.
Harnessing the Bodys Own Signals to Revolutionize Bone Repair
The validation of this hypothesis came from a series of meticulous denervation experiments in mouse models. When researchers surgically or genetically blocked these newly identified command neurons from functioning at a fracture site, the results were definitive and stark. The mice exhibited severely compromised healing, with significant defects in the proliferation of skeletal cells and a failure of stem cells to differentiate into bone and cartilage. This confirmed a direct causative link: the presence and proper signaling of these neurons are not just helpful for bone repair; they are absolutely necessary.
Further analysis of the molecular signals released by these pro-regenerative neurons pinpointed a handful of key players, including transforming growth factor beta 1 (TGFB1) and sonic hedgehog (SHH). However, one signal stood out as particularly critical: Fibroblast Growth Factor 9 (FGF9). Through experiments where the neurons responsible for secreting FGF9 were selectively destroyed, researchers confirmed its essential role. Without this specific neuron-derived signal, the healing process failed. FGF9 was thus identified as the primary paracrine signal—a molecule that acts on nearby cells—that translates the nerve’s command into direct cellular action at the site of injury.
The identification of the neuron-derived FGF9 signaling pathway represents a paradigm shift in orthopedic medicine, offering a highly specific and promising new target for therapeutic intervention. Instead of relying on broad, systemic treatments, future therapies could be designed to precisely amplify or mimic this natural, nerve-driven repair command. This opens the door to developing drugs that directly harness the body’s own regenerative intelligence to promote faster, stronger, and more reliable healing. These advancements would not just be incremental; they would revolutionize how we approach skeletal repair.
The path forward now involves translating these foundational discoveries into clinical applications. The development of therapies that enhance this natural signaling process could dramatically accelerate recovery times and improve the quality of healed bone. Such treatments would be particularly life-changing for the most vulnerable patient populations. The elderly, who face a high risk of debilitating fractures, and individuals with chronic conditions like diabetes or neuropathy, whose compromised nerve function often leads to poor healing outcomes, stand to benefit enormously. By learning to speak the body’s own regenerative language, medicine is poised to significantly improve recovery and restore quality of life for millions.